Перейти к:
Организационная приверженность среднего медицинского персонала: определение понятия и специфика измерений (обзор зарубежных публикаций)
https://doi.org/10.25207/1608-6228-2025-32-5-96-120
Аннотация
Введение. Вопросам организационной приверженности среднего медицинского персонала в российской исследовательской литературе уделяется пока крайне мало внимания. В то же время в зарубежной научной традиции, берущей свое начало с 1960-х гг., приверженность рассматривается как своеобразная «квинтэссенция», комплексно отражающая в себе отношение работников государственного здравоохранения не только к своей организации, но и к своей профессии, работодателю, труду в целом. В этом смысле приверженность выходит за рамки измерений удовлетворенности/неудовлетворенности трудом, лояльности/нелояльности организации, вовлеченности/невовлеченности в ее работу и т. д.
Цель исследования: на основе анализа зарубежных публикаций систематизировать и критически осмыслить основные подходы к пониманию организационной приверженности среднего медицинского персонала, выявить основные этапы развития данной темы в историографии, основные компоненты и механизмы формирования приверженности в медицинских организациях.
Методы. Проблемно-хронологический, сравнительный и критический анализ литературных источников (n = 3808), размещенных в англоязычной текстовой базе данных медицинских и био логических публикаций «PubMed» и выделенных на основании тематического запроса «organizational commitment of nurses» («организационная приверженность медицинских сестер»).
Результаты. Выделены 4 хронологических этапа изучения вопросов организационной приверженности в зарубежной литературе, отличающиеся как по своему содержанию, так и по направленности научных публикаций. На первом этапе (рубеж 1960/1970-х — 1980-е гг.) публикации, как правило, носили описательный характер и касались в основном характеристики обязательств работников по отношению к своим организациям, приверженности этическим моделям поведения и ценностям профессии. В то же время появились первые исследования, призывавшие к разработке «систем объективных оценок программ охраны труда» работников здравоохранения, которые учитывали бы различные аспекты «трудовой жизни», «ролевую неопределенность» и «ролевые конфликты», влияющие на желание работать в медицинской организации. На втором этапе (1990-е гг.) внимание исследователей привлекли вопросы изучения вовлеченности и удовлетворенности трудом как факторов, определяющих организационную приверженность персонала. В публикациях, посвященных анализу «личного жизненного опыта», внедрения психологических контрактов и моделей «совместного управления», создания «самостоятельных рабочих групп медсестер» и «совместных команд», отмечалась необходимость вовлечения среднего медперсонала в управление организациями. На третьем этапе (рубеж 1990/2000-х — начало 2020-х гг.) появилось множество публикаций, посвященных измерению приверженности среднего медперсонала на основе применения модели Дж. Мейера и Н. Аллен. Большое значение приобрел анализ «особости» медсестринского труда в ключе формирования «культуры учреждений», учета ожиданий сотрудников и создания атмосферы воспринимаемой поддержки. В поле зрения оказались вопросы эмоциональных составляющих труда, совмещенные с комплексным изучением проблем эмоционального истощения, стрессов и стрессоров, профессионального выгорания, деперсонализации и пр. При этом наблюдался процесс расширения географии исследований, совмещенный с попытками понять специфику организационной приверженности за пределами «западного опыта». На четвертом этапе (с начала 2020-х гг.) внимание исследователей привлекли вопросы безопасности персонала на рабочих местах, коллективного эмоционального и профессионального выгорания и сохранения «качества здоровья» среднего медперсонала. Новыми темами стали вопросы влияния цифровизации и мультикультурности на поддержание организационной приверженности и стабильности медсестринских коллективов.
Заключение. В дискуссиях по вопросам содержания организационной приверженности и проблемам его качественного измерения рано ставить точку, так как реальная жизнь ставит все новые и новые проблемы, требующие адекватного изучения и детального научного анализа. Результаты обзора позволяют не только совершенствовать существующие подходы к оценке организационной приверженности, но и разрабатывать комплексные программы организационного развития, ориентированные на удержание, мотивацию и профессиональное развитие среднего медицинского персонала в российских медицинских учреждениях.
Ключевые слова
Для цитирования:
Кузьмин К.В., Петрова Л.Е., Харченко В.С. Организационная приверженность среднего медицинского персонала: определение понятия и специфика измерений (обзор зарубежных публикаций). Кубанский научный медицинский вестник. 2025;32(5):96-120. https://doi.org/10.25207/1608-6228-2025-32-5-96-120
For citation:
Kuzmin K.V., Petrova L.E., Kharchenko V.S. Organizational commitment of nursing staff: Definition of the concept and specifics of measurement (review of foreign publications). Kuban Scientific Medical Bulletin. 2025;32(5):96-120. (In Russ.) https://doi.org/10.25207/1608-6228-2025-32-5-96-120
ВВЕДЕНИЕ
Изучение приверженности сотрудников к длительной работе в организации (или — «организационной приверженности»), рассматриваемой в качестве особой эмоциональной (психологической) привязанности персонала к организации (работодателю), поддерживающей вовлеченность и преданность сотрудников и не дающей им возможности либо препятствующей их желанию искать работу в другом месте, является новой для российских исследователей и потому пока не обладает широкой исследовательской базой, выраженной в достаточном массиве прикладных научных публикаций.
Впервые интерес к обозначенной тематике обнаруживается в 2010‑е гг. [1–7], однако фундаментальной можно посчитать статью Ю. В. Потаповой и В. А. Климухиной «Структура и факторы формирования организационной приверженности: теоретическая модель» [8], в которой на основе системного подхода Дж. Мейера и Н. Аллен (1991) [9] представлен анализ факторов формирования и содержательных особенностей компонентов приверженности при соотношении с такими понятиями, как «лояльность работников», «вовлеченность персонала», «удовлетворенность трудом», «организационная идентификация» и др. По определению авторов, высокая приверженность сотрудников к работе в организации порождает множество позитивных последствий, способствуя повышению удовлетворенности работой и уровня доверия организации, производительности труда, мотивации и снижению текучести кадров, стресса и выгорания, возрастанию готовности к внедрению инноваций, повышению оптимизма и улучшению способности справляться с неудачами в профессиональной деятельности и т. д.
При этом важно учесть тот факт, что организационная приверженность — более широкое понятие по сравнению с такими, подчас отдельно изучаемыми, понятиями, как удовлетворенность/увлеченность трудом, вовлеченность в работу организации, лояльность работодателю и пр. Обращаясь именно к объяснительному конструкту «организационная приверженность», мы достигаем комплексного подхода в получении новых знаний о феномене и их использовании для управленческих решений.
Особенно актуален поиск объяснительных моделей поведения сотрудников медицинских организаций — как теоретических, дающих приращение знания о социальных механизмах достижения качества медицинской помощи, так и практических, обладающих потенциалом реальных организационных изменений, так как решение задач здоровьесбережения в рамках достижения национальных целей РФ1 предполагает сохранение населения, укрепление здоровья и повышение благополучия людей за счет повышения доступности медицинской помощи и преодоления как «количественного», так и «качественного» дефицита кадров в здравоохранении.
Понятие «организационная приверженность» в этой связи отвечает, на наш взгляд, указанным задачам — как теоретическим, так и прикладным. При этом важно учитывать, что медицинские сестры — один из центральных элементов системы здоровьесбережения нации — играют ключевую роль в реализации мероприятий по обеспечению эффективности и качественной медицинской поддержки. Тем не менее изучение особенностей организационной приверженности среднего медицинского персонала представлено в российской литературе фактически только одной публикацией — статьей С. В. Умнова и соавт. «Современные подходы к формированию высокой приверженности персонала медицинской организации» [10], в которой авторы выделили 4 основных направления, влияющие на приверженность: 1) сокращение дистанции и изменение корпоративной культуры; 2) повышение функциональной гибкости персонала; 3) создание возможностей для карьеры и профессионального роста; 4) вовлечение персонала в управление.
Цель исследования — теоретический анализ зарубежных публикаций, посвященных концепту организационной приверженности, который в российском контексте здравоохранения представляет собой новый и недостаточно изученный феномен. Теоретические аспекты цели: систематизировать и критически осмыслить зарубежные подходы к пониманию организационной приверженности, выявить ее основные компоненты и механизмы формирования в медицинских организациях. Прикладные цели заключаются в адаптации полученных знаний для дальнейшего развития управленческих практик в российской системе здравоохранения, направленных на повышение мотивации и удержания медицинского персонала, что будет способствовать улучшению качества медицинской помощи и решению кадрового дефицита. Такой подход позволит заложить основу для дальнейших эмпирических исследований и практических рекомендаций в рамках национальных целей развития отрасли здравоохранения.
В исследовании впервые предпринята попытка комплексного анализа имеющихся научных подходов к изучению организационной приверженности среднего медицинского персонала как объяснительной модели и механизма улучшения. Обзор зарубежных публикаций предназначен для обоснованного выбора дизайна эмпирических исследований персонала в российских медорганизациях.
МЕТОДЫ
В исследовании применены качественные методы: проблемно-хронологический, сравнительный и критический анализ. Отбор материалов проводился посредством целенаправленного поиска в англоязычной текстовой базе данных медицинских и биологических публикаций «PubMed» с использованием ключевых слов, релевантных теме организационной приверженности медицинского персонала. Критериями отбора являлись актуальность, полнота раскрытия темы и методологическая достоверность. Анализ литературы осуществлялся поэтапно: после формирования базы данных публикаций были систематизированы основные подходы и теоретические модели, затем проведено сопоставление результатов различных исследований, а в завершающей стадии выполнена критическая оценка и выявление научных пробелов.
Объективность и достоверность интерпретации полученных данных обеспечивались с помощью триангуляции, включающей систематическое сопоставление результатов, полученных разными исследователями, в ходе регулярных обсуждений в авторском коллективе. Такой подход предполагает многогранное рассмотрение материала, что снижает влияние субъективных и методологических искажений. Регулярные совместные обсуждения позволяли интегрировать различные точки зрения, обеспечивая комплексную и надежную интерпретацию результатов исследования.
Авторы использовали наукометрический (количественный) подход в оценке научных публикаций — ниже представлена динамика публикационной активности зарубежных исследователей, что в целом свидетельствует о востребованности объяснительного концепта «организационная приверженность» (рис. 1).
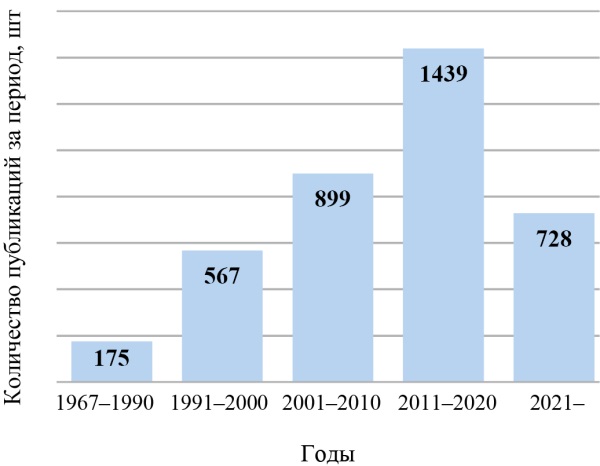
Рис. 1. Количество публикаций (n = 3808)
Примечание: рисунок выполнен авторами.
Fig. 1. Number of publications (n = 3808)
Note: The figure was created by the authors.
В то же время данное исследование представляет собой скорее литературный обзор научных публикаций (метаобзор), нежели наукометрический анализ, что накладывает определенные ограничения на количественную оценку развития научной темы. Однако такой подход позволяет глубоко и критически осмыслить концептуальные основы организационной приверженности, обеспечивая теоретическую базу для последующих эмпирических исследований и практических рекомендаций в сфере здравоохранения.
Всего по тематическому запросу «organizational commitment of nurses» («организационная приверженность медицинских сестер») в базе данных «PubMed» идентифицированно свыше 3,8 тыс. статей2, обращенных к анализу заявленной проблематики.
Очевидно, что интерес исследователей к изучению содержания и специфики измерений организационной приверженности среднего медицинского персонала постоянно растет: если за период с 1967 по 1990 г. вышло 175 публикаций указанной тематики (4,6 % от общего числа), то с 1991 по 2000 г. — 567 (14,9 %), с 2001 по 2010 г. — 899 (26,6 %), а с 2011 по 2020 г. — уже 1439 (37,8 %). Можно предположить, что выявленная динамика сохранится и в дальнейшем; во всяком случае за период с 2021 по март 2025 г. было опубликовано свыше 700 статей; при этом, к сожалению, совсем не представлены исследования российских авторов. Методы: проблемно-хронологический, сравнительный и критический анализ публикаций. Отбор литературы осуществлялся на основании критериев релевантности тематике исследования. Анализ проводился несколькими авторами, что минимизировало субъективность оценок.
РЕЗУЛЬТАТЫ
Как содержательно, так и по качественным характеристикам (новизна результатов) статьи, посвященные анализу организационной приверженности такой специфической социально-профессиональной группы, как медицинские сестры, различаются, что позволило выделить 4 основных хронологических этапа в изучении темы в зарубежной историографии.
1. Начальный этап формирования концепции применительно к изучению среднего медицинского персонала — конец 1960‑х — начало 1990‑х гг.
Первые публикации, увидевшие свет в конце 1960‑х — 1980‑е гг., как правило, носили описательный характер; они касались в основном анализа «обязательств» средних медработников по отношению к своим организациям, коллегам и/или пациентам, «приверженности» этическим моделям поведения, а также роли ценностей профессии в оказании помощи больным людям [11–15].
При этом общей для авторов была убежденность, что социальная значимость профессии и внедренные стандарты оказания медицинской помощи автоматически порождают приверженность организации [16], выраженную в «миссионерском рвении» среднего медицинского персонала в выполнении своего предназначения [17], а личностный и профессиональный рост всегда представлялись производным от приверженности организации [18]. К примеру, утверждалось, что медсестры должны «полностью осознавать, что их профессия подразумевает работу 24 часа в сутки, 7 дней в неделю, включая праздники» [19], так как главным ресурсом развития здравоохранения является «выполнение медсестрами своих обязательств» [20]. K. Zander (1988) [21] указывал, что в основе приверженности лежат ответственность медсестер за результаты ухода за пациентами, «неустанное выражение ухода», «готовность учиться и рисковать», «слушание, отзывчивость, чувство юмора и признание вклада каждого», а D. L. Patterson (1991) [22] — что «приверженность совершенству требует пожизненной приверженности сестринскому делу, исследованиям, обучению, личному балансу и благополучию». Нередко организационная приверженность рассматривалась исключительно в контексте взаимодействия медсестры и пациента, о чем красноречиво свидетельствовал K. Krause (1993) [23], утверждавший, что «профессия не может развиваться без сильной приверженности задаче сестринского дела, эта приверженность и ее совершенствование являются важнейшей задачей. За приверженностью следуют ответственность, коллегиальность и коллективность как средства достижения общей цели».
Если же ничего из вышеперечисленного не наблюдалось, то «корень проблем» виделся в недостаточности либо отсутствии необходимой «биологической» или «медицинской» подготовки медсестер, а также в дихотомии, возникающей между «сестринским образованием и сестринским обслуживанием» [24], выраженной, например, в несогласованности сфер профессиональной подготовки и оказания медицинской помощи [25] и «необученности» ведению необходимой документации [26] и порождающей недовольство и конфликты молодых медсестер при устройстве на работу в больницы.
Иными словами, средний медперсонал рассматривался в первую очередь как объект воздействия со стороны менеджеров больниц, но при этом фактически был лишен права самостоятельного «голоса»; неслучайно в связи с этим впоследствии D. Ouellet и C. Elsner (1993) [27] отмечали, что для понимания природы приверженности необходимо сначала сформировать «профессиональный массив знаний в области сестринского дела и гарантировать, что текущая практика основана на достоверных результатах исследований», а M.C. Corley и H. O. Mauksch (1993) [28] указывали, что истинному пониманию приверженности мешает «переплетение» в образе медсестры «множественности обязательств» — организационных, рабочих, профессиональных, служебных, пациентских и кадровых, за которыми не видно самого предмета, а именно того, чего ожидают медсестры, и как они вообще со своими «обязательствами» справляются. Значительное влияние на ситуацию также оказывало «женское лицо» профессии: организационные структуры и системы, основанные на патриархатных началах, очень часто задерживали или напрямую противодействовали реализации карьерных устремлений медсестер [29].
Первым, кто обратил внимание на оборотную сторону медали, а именно на то, что сама медицинская организация может и должна сделать для удержания у себя среднего медперсонала, стал S. B. Webb Jr. (1975) [30], подчеркнувший важность разработки и внедрения «системы объективных оценок программ охраны труда», основанной на «профессионально приемлемых руководящих принципах и стандартах» и нацеленной не на получение больницами сиюминутной выгоды, а на поддержание здоровья сотрудников и их желания максимально долго работать в здравоохранении. В частности, исследователь подчеркивал, что такая система должна включать в себя 4 компонента: 1) руководящую философию и политику; 2) организационную структуру; 3) ресурсы; 4) службы охраны труда.
Наиболее эффективными средствами разработки таких «систем объективных оценок» исследователи называли:
1) внедрение принципов партисипативного управления3 и фасилитирующего лидерства4 в работу организаторов сестринского дела, способствующих развитию лидерских качеств среди персонала и повышающих его мотивацию и ответственность за счет расширения возможностей высказывать свое мнение и принимать участие в обсуждении ключевых вопросов [31][32];
2) расширение возможностей «совместного управления» сестринским делом с привлечением клинического и управленческого персонала как механизма повышения приверженности организации, ответственности и профессионализма [33];
3) постоянный мониторинг качества сестринского ухода на уровне отдельных подразделений внутри каждой больницы с вовлечением в него всех медсестер [34].
К примеру, позднее T. Porter-O’Grady (1991) [35] замечал, что «переход к совместному управлению влияет на то, как медсестры работают и относятся к организации. Использование стратегий коллективных переговоров, перемещение медсестры в сферы контроля над вопросами, которые учреждения когда-то считали выходящими за рамки ее роли или прав, и стратегии управления конфликтами должны будут измениться, чтобы облегчить перемещение медсестер в основной поток принятия решений. По мере того как учреждение переходит от иерархической структуры к многопрофильной и создается более отзывчивая рыночная организация, медсестрам придется играть более активную роль в маркетинге и управлении своей практикой», а C. Doherty и W. Hope (2000) [36] подчеркивали, что «совместное управление — это культурное изменение, которое будет развивать лидерские и управленческие навыки всех категорий персонала; это не быстрое решение для профессии, [так как] вовлечение всего персонала требует времени, настойчивости, решимости и сильной приверженности обучению и развитию».
Постепенно исследователи начинали также осознавать, что средний медперсонал следует рассматривать в качестве важного и особенного объекта научного изучения: так, на необходимость детального анализа и измерения качества «трудовой жизни» медсестер в связи с организационной и профессиональной приверженностью впервые обратила внимание H. L. Smith (1981) [37], обнаружившая, что наиболее высокие показатели приверженности отмечаются у тех работников, которые сообщают об удовлетворенности трудом, а самые низкие — у тех, кто отмечает у себя высокий уровень «напряженности на работе».
Природа такой напряженности виделась, с одной стороны, в «ролевой неопределенности» — неуверенности средних медработников относительно ожиданий других субъектов (врачей, управленцев, пациентов и пр.), а с другой — в «ролевых конфликтах», возникающих на основе «несовместимых требований от различных отправителей ролей или от нескольких ролей, выполняемых одновременно» [38]. При этом, как замечал M. Jamal (1984) [39], отсутствие приверженности, выраженное в трудовом абсентизме (прогулах, опозданиях и текучести кадров), проистекает из «оцениваемых факторов стресса на работе», включающих в себя «ролевую двусмысленность, ролевую перегрузку, ролевой конфликт и нехватку ресурсов», что неизбежно снижает производительность. Преодолению же «ролевой неопределенности» и повышению приверженности должно служить сочетание автономии (самоконтроля за трудовой деятельностью работника) и социальной интеграции (выстраивания отношений с коллегами) [40].
Помимо этого, также были обнаружены существенные отличия в организационной и профессиональной приверженности медицинских сестер, на что, в частности, одними из первых обратили внимание L. G. Kraemer и J. Rigolizzo-Gurenlian (1985) [41], отмечавшие, что сотрудник нередко вынужден выбирать между профессией и организацией, «поскольку их ценности конфликтуют»: профессионал рассматривается как отвечающий авторитету, основанному на экспертизе, а организация характеризуется авторитетом, основанным на иерархической, в первую очередь бюрократической, позиции. В связи с этим обращалось внимание на этические составляющие приверженности: P. J. Christensen (1988) [42] замечал, что менеджеры здравоохранения должны нести «ответственность за создание этической рабочей среды», включающей в себя «этическую осведомленность, принципиальное обоснование, моральную приверженность профессии и друг другу, а также первоочередное внимание к человеческому благополучию со стратегиями его продвижения», — то есть за все то, без чего формирование приверженности невозможно.
Таким образом, авторы первых исследований, посвященных изучению организационной приверженности среднего медицинского персонала, обратили внимание на две связанные и зависимые друг от друга переменные: «внешнюю», обусловленную необходимостью переосмысления управления сестринским делом в организациях здравоохранения, и «внутреннюю», отмеченную попытками изучить и понять, что может служить стимулами для сотрудников в развитии их заинтересованности в длительной работе в медицинской организации. Неслучайно, суммируя опыт и достижения первых исследований, M. J. Moran и J. E. Johnson (1992) [43] отмечали, что формирование приверженности должно охватывать все уровни структуры организации, и штатная медсестра, наряду с другими специалистами, в том числе управленцами, играет жизненно важную роль, являясь «лучшим человеком для оценки состояния услуг здравоохранения и работы над улучшением процессов, посредством которых эти услуги предоставляются клиентам в условиях здравоохранения».
2. Классический этап моделирования концепции — 1990‑е гг.
Качественно новый этап, в частности, характеризуемый стремлением исследователей понять и детально проанализировать настроения среднего медперсонала в ключе разработки и практического применения новых методик изучения вовлеченности в работу и удовлетворенности трудом, отмечается в 1990‑е гг. Определяющими здесь стали своеобразные «поиски смыслов» — ответов на вопросы, главными из которых стали вопросы о том, что же лежит в основе и какие факторы определяют приверженность среднего медперсонала к длительной работе в медицинской организации?
При этом на первый план вышли призывы, с одной стороны, тщательнейшим образом изучить «личный жизненный опыт» средних медработников для того, чтобы наконец-то четко определить их «роль в творческой и поддерживающей среде», а также особенности профессионального роста и развития [44], а с другой стороны, «внедрить социологию» в исследования в целях создания новой целостной модели сестринского дела, основанной на профессиональной и организационной приверженности, но при этом избавленной от «сомнительного эклектизма, маргинализации философских противоречий и маскировки сложных эпистемологических и онтологических конфликтов» [45].
В частности, одним из первых исследователей, обратившихся к изучению удовлетворенности работой среднего медперсонала на основе массовых опросов, стал M. A. Blegen (1993) [46], выделивший 7 переменных, оказывающих наибольшее воздействие на формирование приверженности к длительной работе в медицинской организации, а именно: общение с руководителем, автономия, признание, рутинизация (стандартизация должностного функционала), общение с коллегами, справедливость и «локус контроля» — степень, в которой сотрудники верят, что они, в отличие от внешних сил (вне их влияния), контролируют исход событий в своей жизни. В свою очередь, S. Acorn et al. (1997) [47] отмечали, что, хотя удовлетворенность трудом является предиктором (предвестником/маркером) организационной приверженности, все же наиболее важной нужно считать децентрализацию работы с четким определением обязанностей, функций и прав медсестры, поскольку именно децентрализация «влияет на организационную приверженность как напрямую, так и косвенно, через профессиональную автономию и удовлетворенность работой». Целый ряд авторов [48–51] подчеркивал, что важнейшими факторами, обеспечивающими приверженность, удовлетворенность работой и качество принимаемых решений, являются сплоченность коллектива, открытое обсуждение возникающих трудностей в процессе как формального, так и неформального общения, а также поддержка со стороны менеджеров и всего персонала, в том числе и немедицинского.
Тем самым ставился вопрос о необходимости кардинальных организационных перемен в работе как медицинских организаций в целом, так и их руководителей/менеджеров, врачебной и медсестринской корпораций. Симптоматичным в связи с этим стало появление исследований, посвященных проблемам внедрения неформальных «психологических контрактов» между работодателями и сотрудниками, основанных на их ожиданиях друг от друга «с точки зрения работы и организационных обязательств», поддержании взаимного доверия и достижении взаимовыгодных соглашений «по всем вопросам, где это возможно»; к примеру, S. J. Cavanagh (1996) [52] подчеркивал, что «психологический контракт — это неявное соглашение между работодателем и сотрудником о том, что каждая сторона будет относиться к другой справедливо… Хотя такой контракт не является юридически обязывающим соглашением, он, тем не менее, является обязательным соглашением между людьми». Сходным образом рассуждал A. E. Molzahn (1997) [53], полагавший, что важнейшим средством формирования приверженности является внедрение новой, «заботливой», организационной культуры, важнейшими составляющими которой должны стать «ценности группы, качества заботливого лидера, стиль управления, процессы принятия решений, планирование изменений, принятие мер и размышление/оценка/ответственность».
При этом исследователи предлагали различные варианты формирования «заботливой культуры». Так, I. Johansson et al. (1994) [54] подчеркивали определяющую значимость межличностных отношений и фасилитирующего лидерства руководителей медсестринских коллективов, а G. MacDonald (1995) [55] — необходимость внедрения «совместного управления», реализуемого на корпоративной основе и способного «повысить вовлеченность медсестер в работу, мотивацию, качество трудовой жизни, организационную приверженность, возможность влиять на уход за пациентами и профессиональную гордость». M. C. Narayan et al. (1996) [56], F. Annand (1997) [57] и M. Parker и S. Gadbois (2000) [58] ратовали за создание «самостоятельных рабочих групп медсестер» («сообществ на рабочем месте»), разрабатывающих конкретные вопросы управления на уровне отдельных подразделений и основанных на принципах наставничества, общения, организационной приверженности, сотрудничества и совместного вклада в общее дело; C. K. Wilson (1998) [59] — за создание «совместных команд», объединяющих менеджеров и специалистов сестринского дела и основанных на взаимозависимости, организационной власти, самоопределении, компетентности, приверженности и «подлинной заботе о качестве выполняемой работы»; M. A. McCrea (1998) [60] — за установление «баланса сил», обеспечивающего приверженность всех заинтересованных сторон настоящему партнерству и совместное участие в принятии решений.
Отдельное внимание было уделено критическому анализу состояния межличностных и профессиональных взаимодействий на уровне медицинских организаций. Например, S. Makaram (1995) [61] называл фактором, существенно снижающим организационную приверженность, «исторически» конфликтные отношения медсестры и врача, порождающие дисбаланс в деятельности организаций и мешающие межпрофессиональному сотрудничеству, а D. Corrales et al. (2000) [62] в связи с этим подчеркивали, что зачастую взаимодействие врачей и медсестер строится на уровне взаимных обвинений, так как «врачи считают, что медсестры не хотят брать на себя совместную ответственность за рабочую нагрузку в медицинских центрах, а медсестры считают, что врачи не хотят делиться задачами, а скорее [их] делегируют или приказывают им». Подобная «обвинительная риторика» сохранится и в дальнейшем: например, L. Caricati et al. (2014) [63] отмечали, что «профессиональная приверженность врачей препятствует их готовности сотрудничать с медсестрами таким образом, чтобы признавать их автономию» и если медицинские сестры всегда готовы к таком сотрудничеству, то врачи, как правило, его необходимость начисто отрицают.
В свою очередь, A. M. Brewer и P. Lok (1995) [64] подчеркивали, что в отсутствии доверия и организационной идентификации виноваты прежде всего сложившиеся неравноправные отношения между медсестрами и руководством больниц, так как последнее чаще всего присушивается к мнению врачей, но не медсестер, а R. B. Dwore et al. (2000) [65] упрекали управленцев в том, что те искусственно поддерживают «стеклянный потолок», не давая медсестрам продвигаться на управленческие должности и сознательно рассматривая их в роли работников «второго сорта».
В связи с вышесказанным авторы публикаций указывали на противоречия, сложившиеся внутри самой культуры медицинских организаций: с одной стороны, приверженность виделась как результат конструктивного сотрудничества всех заинтересованных сторон, ядром которого является пара «врач-медсестра» [66], а с другой — именно медсестры являются первыми, кого не хотели бы видеть в качестве равноправных партнеров, участвующих в обсуждении вопросов состояния и перспектив развития медицинских организаций, ни врачи, ни управленцы [67]. Неслучайно B. D. Gifford et al. (2002) [68] подчеркивали, что «бюрократическая культурная норма больниц с ее иерархическими структурами, правилами и положениями, а также сильным акцентом на измерении результатов и затрат, возможно, не является культурой, наиболее благоприятной для повышения удовлетворенности работой и приверженности медсестер».
Предметом изучения исследователей 1990‑х гг. также стали факторы, мотивирующие средних медработников оставаться в организации на длительный срок: например, R. Bergler (1995) [69] замечал, что такая мотивация «в первую очередь носит личный характер», включая в себя «социальную приверженность, мотивацию к достижению и ответственность за решение разнообразных человеческих проблем»; демотивирующими факторами становятся пренебрежение пациентами, стресс, дезорганизация рабочего времени, засилье бюрократии и отсутствие личной ответственности.
Особое внимание уделялось эмоциональным (аффективным) составляющим организационной приверженности, присущим в целом профессиям, относящимся к типу «человек—человек». В частности, отмечалось, что состояние «профессионального психического здоровья» является определяющим фактором, стимулирующим рост производительности среднего медперсонала, повышение приверженности и удовлетворенности работой [70], а в основе его поддержания лежат способности анализировать причины и интенсивность стрессов, адекватно реагировать на стрессоры, а также нейтрализовывать их ожидаемые негативные последствия [71]. Укреплению психического здоровья должно также содействовать развитие культуры толерантности, нацеленной на необходимость учета при планировании и внедрении стратегий управления и лидерства «культурного многообразия» [72], так как сама «пациентская среда» заставляет практикующих медсестер чаще задумываться о ценностях и приверженности профессии, находя себя в принятии «иных» пациентов, сочувствии и «демонстрации этноцентричности» [73].
В целом на важность анализа качеств «среды ухода за пациентами» указывал S. H. Pappas (1995) [74], отмечавший, что приверженность становится результатом как способностей медсестер «предоставлять качественную помощь пациентам и получать личное удовлетворение от работы по уходу», так и их «выносливости», включающей в себя 3 важнейшие характеристики: 1) веру в то, что люди могут контролировать или влиять на события в своей жизни; 2) способность чувствовать себя вовлеченными в профессию; 3) ожидание перемен как «захватывающего вызова для дальнейшего развития». Однако, как указывали пессимистически настроенные авторы [75], в условиях хронической нехватки персонала такое вряд ли возможно, и, учитывая тот факт, что удовлетворенность пациентов является ключом к пониманию удовлетворенности медсестер своей работой, без адекватного кадрового обеспечения сформировать их высокую организационную приверженность не получится.
При этом показательным оказывался тот факт, что обсуждение проблем организационной приверженности и алгоритмов ее формирования вызывало серьезную настороженность, а подчас — негодование со стороны приверженцев «старой» школы сестринского дела5. Например, V. M. Woodward (1997) [76] указывал на риски разрушения «целостности целого» — экспрессивных компонентов сестринской деятельности, основанных на альтруистических ценностях; M. B. Modic и M. Amour (1998) [77] призывали «вернуть» в сестринское дело приверженность профессии, а не организации; C. L. Farley (2003) [78] — заменить абстрактную и малопонятную приверженность «обучением служению», охватывающим широкий спектр всех видов практической деятельности и медицинской педагогики; J. Salvage (1998) [79] — прекратить смешивать «альтруизм и прагматизм», пытаясь прикрыть попытки «контролировать медсестринскую профессию» повышением приверженности организации. Наконец, M. H. Hem и K. Heggen (2004) [80] указывали на то, что приверженность, основанная на организации повседневной работы в больничном отделении, четком разделении труда между медсестрами и врачами и прагматичном подходе медсестер к уходу за больными, вообще противоречит главной сестринской ценности — состраданию.
Организационной приверженности нередко противопоставлялась приверженность профессии: к примеру, B. Beagan и C. Ells (2009) [81] утверждали, что средние медработники в подавляющем своем большинстве выражают «приверженность ценностям помощи другим, заботе, ориентированности на пациента, защите его интересов, профессиональной честности, целостному уходу и обмену знаниями для расширения прав и возможностей пациентов», но, сталкиваясь с политикой внедрения организационных ценностей, они зачастую испытывают проблемы и разочарование, испытывая растущее давление профессиональных иерархий и властных структур.
И все же в целом организационная приверженность среднего медперсонала стала с 1990‑х гг. рассматриваться как один из важнейших элементов, обеспечивающих «удовлетворение потребностей и предпочтений пациентов, особенно в областях эмоциональной поддержки, координации ухода, подготовки к выписке и вовлечения семьи и друзей», наряду с инвестициями в обучение и переподготовку персонала, перепроектированием систем оценки его работы, мероприятиями по повышению качества лечения и сестринского ухода, обеспечением «коммуникации между лицами, осуществляющими уход, пациентами и членами их семей» [82]. Неслучайно R. A. Westrope et al. (1995) [83] подчеркивали, что «качественный уход за пациентами лучше всего обеспечивают компетентные клинические сотрудники, которые преданы своей работе, организационным ценностям и целям и сохраняют занятость с течением времени», а R. Peterson (1999) [84] отмечала, что обеспечение качественного ухода за пациентами немыслимо вне «собственного профессионального роста» среднего медперсонала, так как именно медсестры уполномочены быть «заботливыми целителями, учителями и защитниками интересов пациентов в постоянно меняющейся среде здравоохранения».
3. Прикладной этап «внедрения социологии» в сестринские исследования — рубеж 1990/2000‑х — начало 2020‑х гг.
Новый содержательный поворот в исследованиях обнаруживается на рубеже 1990/2000‑х гг., что можно связать с попытками комплексного анализа особенностей организационной приверженности среднего медперсонала. При этом основными задачами стали, с одной стороны, изучение путей преодоления противоречий между профессиональной и организационной приверженностью, проявляющих себя, в частности, в стремлении к идеалу индивидуализированной целостной помощи и реальностью среды с ограниченными ресурсами [85], а с другой стороны, детальный критический анализ специфики коммуникаций, приверженности, вовлеченности, достижения консенсуса и совместимости действий разных субъектов здравоохранения, обеспечивающих комплексный уход за пациентами и помощь их близкому окружению [86].
Одними из первых здесь стали P. J. Kalbfleisch и B. W. Bach (1998) [87], утверждавшие, что ожидаемые размеры адекватного вознаграждения способствуют росту организационной приверженности, удовлетворенности и вовлеченности в работу; при этом факторами, провоцирующими снижение приверженности, назывались сверхнапряжение на работе, отсутствие внимания со стороны окружающих, частая и необоснованная критика, а также редкость или несоразмерность затраченному труду вознаграждений. При этом целый ряд исследователей [88–91] отмечал, что для повышения приверженности необходимо внедрить программы удержания/сокращения текучести кадров, вознаграждения/признания и ротацию рабочего графика и обязанностей, так как основными причинами, по которым медсестры меняют работу, являются недовольство размерами зарплаты, объемом нематериальных льгот и графиком работы, а также «воспринимаемые» организационные стрессы, связанные как с уходом за пациентами, так с взаимодействием с начальством и коллегами, проявляющиеся в ухудшении здоровья сотрудников, вызывающие профессиональное выгорание и «моральное возмущение» и способствующие как уходу из организации, так и уходу из здравоохранения в целом.
Напротив же, когда руководители организаций и средний медперсонал находятся «в одной лодке» и понимают свою «взаимозависимость», тогда у сотрудников формируется позитивное организационное мышление, основанное на принципах партнерства, автономности и «гордости за организацию», а их вовлечение в совместную постановку целей, организованную вокруг «наших проблем», а не собственных забот руководителя, ведет к формированию длительной привязанности к организации [92]. При этом, по утверждению M. Simons (2004) [93], формирование высокой приверженности в принципе невозможно без ответной приверженности руководителей медорганизаций благополучию сотрудников, основанной на принципах «заботливой и сострадательной культуры»: «Так же, как мы заботимся о тех, кто находится в наших стенах, мы должны планировать и реализовывать программы, которые способствуют здоровью и благополучию нашего сообщества».
По мнению исследователей, на приверженность среднего медперсонала влияют не только воспринимаемый «имидж работы» и напряжение, с ней связанное, но и завышенные/необоснованные требования со стороны пациентов, их родственников, врачей и менеджеров [94], провоцирующие стрессы, выгорание, эмоциональное истощение, деперсонализацию и психосоматические проблемы со здоровьем, в конечном счете выливающиеся в выраженное стремление «порвать с организацией» [95][96]. Для преодоления негативных последствий «эмоционального истощения» и в целях создания оптимальной «заботливой среды» предлагалось широко использовать возможности социокультурной анимации — организации «зон спокойствия», проведения регулярных развлекательных мероприятий, назначения лиц, ответственных за противодействие издевательствам и непрофессиональному поведению, неформального признания заслуг и пр. [97].
При этом D. K. McNeese-Smith (2000) [98] одной из первых призвала рассматривать организационную приверженность во временном диапазоне, то есть в зависимости от стажа работы и возраста медсестры, отметив, что ее величина будет зависеть от того либо иного этапа карьерного роста и профессиональных изменений в сознании сотрудника, связанных с особенностями личностной идентификации с «рабочей средой» в организации. Исследователь выделила 3 этапа: вхождение в организацию («вступление в должность»), достижение мастерства («освоение должности») и отстранение от организации («выход из должности»), отметив, что чем дольше медсестра работает в организации на одной должности, тем больше она «отстраняется от нее», и состояние приверженности в итоге сменяется состоянием «разъединения». Наибольшую же удовлетворенность работой, производительность и организационную приверженность демонстрируют медсестры старшего возраста, находящиеся на стадии «освоения должности» и имеющие перед собой четкие карьерные перспективы, что подчеркивает «настоятельную необходимость для медсестер и организаций совместно планировать карьеру» [99]. В противовес данным утверждениям M. Ruokolainen et al. (2014) [100] отмечали, что «возрастные» медсестры с большим стажем и опытом работы, будучи наиболее преданными своей организации, более всего уязвимы в неуверенности в своей работе в силу возрастания конфликтов между работой и семьей; молодые же медсестры, чувствующие тесную привязанность к своей организации, используют ее в качестве «защитного фактора» в преодолении неуверенности при выполнении своих должностных обязанностей.
Попытки обнаружить зависимость между приверженностью, возрастом и стажем работы породили в дальнейшем очень интересную дискуссию, связанную с изучением поколенческих различий разных отрядов среднего медперсонала. Так, к примеру, J. Hu et al. (2004) [101] утверждали, что разные поколения («молчаливое», бэби-бумеры, поколения X и Y) вообще «имеют совершенно разные требования к трудоустройству и разные потребности в ориентации, обучении, продвижении по службе, льготах, привилегиях и вариантах выхода на пенсию». Такие требования и потребности, по мнению исследователей [102–104], должны наконец-то заставить медицинские организации и их руководителей научиться «предвидеть межпоколенческие различия» с тем, чтобы «обеспечить благоприятную рабочую среду, признающую эти различия», выработать более дифференцированный «индивидуальный стиль», интуитивно учитывающий мнения разных поклонений, а также понять, что «многообразие поколений на рабочем месте открывает более широкие возможности для практики, поскольку опыт и знания каждого поколения в сестринской среде создают атмосферу принятия и гармонии, способствующую удержанию медсестер». Более того, D. K. McNeese-Smith и M. Crook (2003) [105] полагали, что если организаторы сестринского дела и менеджеры больниц не будут иметь четких представлений о специфике и разнообразии личных ценностей средних медработников в зависимости от их возраста, пола, стажа, этнической, религиозной и поколенческой принадлежности и о том, насколько эти ценности соответствуют или не соответствуют (а, может быть, противоречат) ценностям организации, то разговоры о формировании приверженности организации будут вообще лишены всякого смысла.
Авторы публикаций [106][107] призывали руководителей медсестринских коллективов и больниц при формировании «культуры учреждений», поддерживающей традиции сестринского дела, стремиться к всеобъемлющему «пониманию нужд и чаяний» среднего медперсонала, возникающих в связи и по поводу работы, так как в противном случае кадровые потери будут необратимыми: сотрудники, испытывающие потерю идентичности и смысла в работе, отреагируют на все это «в форме ухода, изоляции, неудач в командной работе и высокой конфликтной среды». Примечательным в этой связи стало исследование «неоднозначности ролей», проведенное M. Kroposki et al. (1999) [108] и показавшее, что сотрудники, испытывающие сильные конфликты, демонстрируют значимо меньшую организационную приверженность и удовлетворенность работой.
Именно приверженность, доступные ресурсы и поддерживающая организационная среда представлялись важнейшими факторами, обеспечивающими включенность персонала в «культурные нормы организации», находящими свое наиболее яркое отражение как в улучшении качества оказания медицинской помощи [109], так и в нахождении «точек соприкосновения» с ожиданиями сотрудников, связанными с управлением и повышающими такие ценности, как доверие, уважение, приверженность, личные инвестиции и командная работа для достижения целей организации [110], а также в создании «атмосферы воспринимаемой поддержки» в виде неформальных «социальных сетей», объединяющих рядовых сотрудников и руководителей медсестринских коллективов [111].
При этом E. Manias et al. (2003) [112] подчеркивали необходимость создания «эффективных сетей коммуникации», основанных на заинтересованном обсуждении всеми сторонами таких вопросов, как «уведомление о наличии смен, распределение работы и признание медсестры как ценного члена команды здравоохранения» и др. В целом же позитивно воспринимаемая в сознании сотрудника «рабочая среда», обеспечивающая равный доступ к информации, поддержке, ресурсам и возможностям учиться и развиваться, активно влияет на отношение сотрудников к работе, производительность и организационную эффективность [113], а «объединение в команды» способствует росту приверженности и «взаимного желания» работать над общей миссией организации и ее видением [114]; при этом важным условием повышения эффективности работы таких команд становится выявление и поддержка неформальных целеустремленных лидеров сестринских коллективов, искренне болеющих за процветание своей организации [115].
В условиях хронического недофинансирования здравоохранения и кадрового дефицита исследователи были убеждены, что формирование новой «культуры учреждений» перебросит «мостик» между «старой приверженностью» мастерству и альтруизму, основанной на защите интересов пациентов и правах человека, и «новой приверженностью», соединенной с ценностями свободы выбора профессии и образа жизни, личной ответственности, понимания вероятных результатов деятельности и «пределов успеха», основанных на справедливом перераспределении ресурсов [116]. Ведущая роль здесь отдавалась всемерному расширению прав и возможностей медсестер, важнейшими элементами которых становились удовлетворенность работой и организационная приверженность [117]; при этом медсестры с большей вероятностью будут удовлетворены и преданы своей профессии, если «они почувствуют, что их мнение услышано и что их рабочая среда способствует профессиональному росту» [118].
Как утверждали J. Motwani et al. (1999) [119], ключевыми компонентами успешности внедрения «культуры учреждений» могут стать: 1) организационная структура и приверженность выявлению и улучшению процессов ее функционирования; 2) использование статистических и аналитических инструментов на основе данных опросов персонала; 3) наделение сотрудников полномочиями брать на себя ответственность за выполнение своих рабочих задач таким образом, чтобы поощрять их непрерывное обучение; 4) вовлечение «внутренних и внешних клиентов» в процессы организационных улучшений; 5) разработка практических мер для мониторинга эффективности внедряемых улучшений. Наконец, кроме всего вышеперечисленного, по мнению B. Hannigan и P. Burnard (2000) [120], медсестры должны обладать «политической осведомленностью», необходимой как для понимания сущности структурных и идеологических факторов, лежащих в основе политики в области здравоохранения, так и для продуцирования собственных политических инициатив.
Следует заметить, что только в 2000–2010‑е гг. исследователи, наконец, обратили внимание на возможности применения модели Дж. Мейера и Н. Аллен для изучения различных типов организационной приверженности, формируемых у среднего медицинского персонала: аффективного, инерционного и нормативного, косвенно доказав, что само по себе «внедрение социологии» в контекст «сестринских исследований» оказалось не такой уж простой задачей. При этом, по образному выражению R. M. Caine и H. Lowenstein (2000) [121], для того чтобы медицинским организациям выжить и процветать «в блуждающих полях напряженных ожиданий, путешествующих по неясным тропам, манипулирующих волшебными технологиями и сталкивающихся с новыми врагами», нужно иметь «мозги, сердце и мужество», а именно приверженность, командную работу и вовлеченность среднего медперсонала.
Пионерами здесь стали S. L. Wagner и M. C. Rush (2000) [122], указавшие на то, что приверженность, удовлетворенность работой и доверие руководству проще и быстрее сформировать у молодых сотрудников, получивших соответствующую поддержку в медицинской организации, и тем самым косвенно подметив, что у медсестер старших возрастов в большей степени превалирует не аффективная, а нормативная приверженность. T. Murrells et al. (2008) [123], в свою очередь, подмечали, что молодые медработники в целом в большей мере подвержены воздействиям, направленным на формирование аффективной приверженности, будучи заинтересованными в содержании работы, направленной на оказание помощи, и благоприятном климате в своем отделении, даже при недостаточности материального вознаграждения.
H. K. Laschinger et al. (2000, 2001) [124][125] предполагали, что более высоким уровнем организационного доверия и аффективной приверженности обладают медсестры, наделенные властными полномочиями; тем самым создание благоприятной среды, усиливающей восприятие расширения прав и возможностей для средних медработников, оказывает положительное влияние на членов организации, повышая ее эффективность, так как «медсестры с более высоким уровнем профессиональной нагрузки значительно более самостоятельны, более преданы организации и более удовлетворены своей работой». Неслучайно, по утверждению L. Kuokkanen и J. Katajisto (2003) [126], при формировании приверженности ведущая роль, наряду с удовлетворенностью работой и ясными возможностями дальнейшего обучения, принадлежит субъективному осознанию работником своей карьеры в конкретной медицинской организации.
Однако приверженность оставаться в организации будет исключительно инерционной при отсутствии других возможностей трудоустройства; в частности, на негативное воздействие «отсутствия обучения, признания и справедливости, неадекватных денежных льгот, плохих отношений с коллегами, этапа завершения карьеры и отсутствия гарантий занятости» обращал внимание D. K. McNeese-Smith (2001) [127]. С другой стороны, медицинские организации, стремящиеся сохранить кадры любой ценой и для этого предлагающие работникам относительно высокие зарплаты и нематериальные льготы, но ничего не делающие для укрепления организационного доверия работников и формирования соответствующей «культуры организации», заведомо рискуют, так как «покупка рабочей силы» порождает цинизм и прагматизм среднего медперсонала по отношению как к выполнению своих обязанностей, так и взаимодействию внутри коллектива [128]. Неслучайно C. P. Hsu et al. (2015) [129] подтверждали, что, хотя вознаграждения и играют важную роль в повышении удовлетворенности работой, их значимость существенно ниже, чем развитие доверия и взаимной поддержки как в коллективе, так и во взаимоотношениях руководителей и их подчиненных.
Впоследствии подобных исследований, основанных на анализе данных социологических опросов среднего медицинского персонала, а также кадровой статистики, и связанных с выявлением положительных либо отрицательных корреляций между организационной приверженностью, удовлетворенностью трудом, вовлеченностью в работу, воспринимаемой доступностью профессионального переобучения, размерами вознаграждения и социальных льгот и текучестью кадров, между намерением покинуть организацию и намерением покинуть профессию, между состоянием воспринимаемого благополучия и проблемами со здоровьем и пр., становится очень много (см., напр., [130–142] и мн. др.). Более того, выводы исследователей нередко оказывались несовместимыми друг с другом, что было связано как с различиями и особенностями изучаемого контингента, так и с разными методологическими подходами к его изучению. Неслучайно нередкими в подобных публикациях оказывались утверждения о том, что для дальнейшего уточнения данных необходимы дополнительные исследования, что «результаты имеют ограниченную обобщаемость… и будущие исследования могут быть направлены на другие объективные измерения производительности» [143].
Некоторые авторы стремились максимально расширить зону исследовательского поиска, пытаясь учесть и измерить наибольшее число факторов, влияющих на приверженность организации и текучесть кадров. К примеру, S. S. Han et al. (2009) [144] выделили 12 таких факторов, в том числе самоэффективность, эффективность работы медсестры, удовлетворенность работой, приверженность организации, стресс, выгорание, организационную культуру сестринского дела, продолжительность обучения в колледже и на рабочем месте, количество больничных коек, стаж работы в здравоохранении и продолжительность работы на текущем рабочем месте; S. A. Vagharseyyedin (2016) [145] на основе комплексного обзора литературы выделил 63 фактора, определяющих организационную приверженность медсестер, разделив их на 4 большие группы: 1) личные характеристики и черты характера медсестер; 2) стиль и поведение руководства и управления; 3) восприятие организационного контекста; 4) характеристики работы и рабочей среды. Без сомнения, в связи с этим попытки сопоставления и нахождения логических связей между множеством факторов, а также противоречий, лежащих в основе их взаимодействий и взаимовлияний, нередко оказывались непосильной задачей для исследователей.
В то же время многие авторы подчеркивали, что, анализируя организационную приверженность среднего медицинского персонала, следует в первую очередь учитывать сам объект изучения, так как медсестринская деятельность обладает значимой спецификой, отличающей ее от иных видов профессиональной деятельности, и, стало быть, невозможно механически перенести традиционное понимание приверженности на средний медперсонал без его досконального и критического изучения в связи с особенностями данной социально-профессиональной группы. При этом в вопросах того, что же в первую очередь формирует у среднего медперсонала приверженность организации, исследователи, хотя и замечали, что «проактивная политика удержания, ориентированная на потребности медсестер, демонстрирует приверженность и заинтересованность в сохранении их на рабочих должностях и в профессии» [146], высказывали самые разные, подчас малосовместимые, предположения.
Например, A. Sjöberg и M. Sverke (2000) [147] замечали, что «намерение текучести кадров опосредует аддитивные и мультипликативные эффекты вовлеченности в работу и организационной приверженности на фактическую текучесть кадров»; иными словами, при анализе показателей вовлеченности и приверженности следует учитывать наличие «промежуточных связей», имеющих отношение не только к организации, но и к медсестринской корпорации в целом, профессии и/или пациентам, а также к уникальным характеристикам «эмоционального труда». Неслучайно M. T. Mrayyan (2008) [148] сообщал, что медсестры нередко оставались на работе в своей организации, даже когда «эта работа не соответствовала их ожиданиям», а, по мнению S. R. Liou (2009) [149], при прогнозировании намерений медсестер уйти из организации необходимо сочетать приверженность, опыт работы, характеристики и условия труда в контексте комплексного анализа личных качеств сотрудников.
Ряд авторов полагал, что следует сосредоточиться на анализе влияния на организационную приверженность таких факторов, как организационная справедливость, организационное доверие и организационная идентификация: например, S. Y. Chen et al. (2015) [150] замечали, что организационная справедливость, позитивно воспринимаемая медсестрами, влияет на их организационные доверие и идентификацию, а последние в конечном счете формируют организационную приверженность. Особую роль играет восприятие получаемой организационной справедливости на неформальном уровне: к примеру, H. Sveinsdóttir et al. (2016) [151] указывали, что медсестры, «часто» получавшие словесную похвалу руководства, показывали большую удовлетворенность работой, описывали более позитивный рабочий климат и были более преданы организации, гордясь тем, что они в ней работают. При этом важнейшим требованием к руководителям называлось «сдерживание обещаний»: «Менеджеры должны быть осторожны, давая только те обещания, которые они могут выполнить, и особенно избегать разрыва психологического контракта», так как невыполненные обещания могут разом «свести на нет» многолетние усилия по формированию приверженности персонала [152].
С другой стороны, исследователи утверждали, что наиболее точными и адекватными в оценках могут быть только пациенты и их близкие: если медсестра оказывает помощь, ориентированную на пациента и связанную с его потребностями, заботится о его чаяниях и тревогах, то она тем самым демонстрирует свою вовлеченность в работу и приверженность организации; «безличный» и «рутинный» уход, лишенный учета индивидуальности больного человека, наглядно представляет собой обратную картину [153]. По утверждению E. Endo et al. (2005) [154], вступая «в заботливые отношения распознавания образов пациентов», медсестры ощущают неизбежные трансформации, преобразующие их сознание и глубоко проникающие во всю сферу сестринской практики; иными словами, медицинская сестра, пронизанная идеями сострадания и преданности профессии, контактируя с больными людьми и их близкими, начинает ощущать неразрывную связь со своей медицинской организацией. Тем самым организационная приверженность автоматически порождается приверженностью профессии, и в большинстве случаев медицинским организациям следует исходить из принципа «один размер подходит всем», направляющего медсестер на прогресс в режиме «синхронизированного шага» в приобретении навыков и знаний в рамках своей специальности [155][156].
И все же целый ряд исследователей критически относился к самому понятию «организационная приверженность»: например, S. De Gieter et al. (2011) [157] вообще отрицали ее роль при принятии работником решения покинуть организацию, так как куда большую роль играют различные аспекты удовлетворенности/неудовлетворенности работой, а M. Cleary и J. Horsfall (2014) [158] полагали, что воспитание приверженности за счет включения медсестер «в иерархическую бюрократическую организацию» способно привести к тому, что те, у кого были «самые заветные позитивные ценности ухода за пациентами, у кого [была] более сильная приверженность моральным убеждениям относительно общественного блага и четко развито понимание параметров целостности, уйдут и, возможно, оставят профессию».
Как и в более ранних исследованиях, большое внимание уделялось «эмоциональным составляющим» труда среднего медперсонала и их влиянию на приверженность организации, однако качественно новыми здесь стали попытки анализа особенностей взаимопроникновения и взаимовлияния, с одной стороны, «эмоционального истощения», «стресса и стрессоров», «профессионального выгорания», «деперсонализации» и пр., а с другой — организационных обязательств, социальной поддержки, способностей к совладанию с трудностями, самоэффективности и т. д.
Так, T. Huynh et al. (2008) [159] отмечали, что «эмоциональный труд» — это процесс, в ходе которого медсестры принимают «рабочую персону» для выражения своих автономных, поверхностных или глубоких эмоций во время встреч с пациентами, включающий в себя 3 важнейших элемента: 1) «организацию» — социальные нормы и социальную поддержку; 2) «медсестру» — идентификацию роли, профессиональную приверженность, опыт работы и межличностные навыки; 3) «работу» — автономию, степень эмоциональной потребности, частоту взаимодействия и сложность профессионального труда. В этой связи если сотрудники «чувствуют себя бессильными», не имея никакого влияния на свою работу, и/или «чувствуют себя бессмысленными», понимая, что их работа не стоит затрачиваемых усилий, то обесценивается не только смысл работы, но «растворяется в воздухе» приверженность организации [160].
При этом P. S. Pendry (2007) [161] сообщала, что нередко медсестры испытывают выраженный «моральный дистресс» — физические или эмоциональные страдания, когда, «имея больше ответственности, чем полномочий, но не имея автономии, чтобы делать то, что, по их мнению, должно быть сделано», они в большинстве случаев уходят и из организации, и из профессии. Интересны в этом отношении данные исследований A. Yildirim и D. Yildirim (2007) [162] и D. Yildirim (2009) [163], изучавших проявления «моббинга» на рабочем месте, включающем в себя эмоциональное давление, запугивание, унижение и «психотеррор» и определяемый как «систематическое, направленное, неэтичное общение и антагонистическое поведение со стороны одного или нескольких лиц»; «травля на рабочем месте» («буллинг») в подавляющем большинстве случаев приводила к депрессии, снижению мотивации, способностей концентрироваться на работе, низкой производительности и плохим отношениям с пациентами, руководителями и коллегами.
Неслучайно в связи с этим L. Olender-Russo (2009) [164] полагал, что «нездоровые отношения между коллегами», выходящие за рамки случайной невежливости и на самом деле направленные на «причинение вреда», являются главными причинами деградации медицинских организаций, приводящими к тому, что «медсестры покидают пункты оказания помощи», а R. Schalk (2011) [165] утверждал, что косвенным подтверждением кризиса приверженности работников своим организациям служит резкий рост числа жалоб на здоровье и невыходов на работу по болезни.
Именно поэтому, по мнению исследователей [166][167], высокий уровень организационной приверженности, проявляющий себя в целенаправленно сформированной профессиональной и личной самоэффективности работника, наличии индивидуальных моделей преодоления трудностей и способностях к самоконтролю, приводит к меньшему выгоранию и значимо меньшей подверженности стрессам, а важнейшую роль в ее укреплении играет «чувство согласованности» жизни самих медсестер как «глобальная ориентация на то, чтобы рассматривать жизнь как структурированную, управляемую и значимую, а также иметь возможность справляться со стрессовыми ситуациями» [168].
Немалую роль в удержании персонала и поддержании высокой приверженности организации играет «воспринимаемая поддержка» со стороны руководства [169], находящая свое отражение в мероприятиях, направленных на преодоление «ролевого стресса».
К примеру, W. H. Ho et al. (2009) [170] и S. Y. Chen et al. (2015) [171] полагали, что при выявлении такого стресса, спровоцированного рутинностью трудовых операций и инерционностью труда, необходимо применять политику «ротации работы», например переводя сотрудников из одного отделения в другое, вовлекая их в смену профессиональных занятий, предлагая аналогичные должности в других подразделениях больницы и т. д.; подобная ротация, по мнению авторов, успокаивающе воздействует на психику работников, косвенно влияя на удовлетворенность работой и оказывая положительное воздействие на приверженность организации, что, в свою очередь, «ограничивает порочный круг высокой текучести кадров и низкого морального духа в организациях, приводящих к растрате ценных человеческих ресурсов». В свою очередь, D. E. Allen et al. (2009) [172] считали, что для профилактики возникновения стрессовых ситуаций на работе и намерений сотрудников уйти из организации необходимы постоянные (ежедневные или еженедельные) неформальные собрания руководителей и коллектива, организуемые в одно и то же время для свободного обсуждения «рассказов» сотрудников о беспокоящих их проблемах как на работе, так и в личной/семейной жизни в поддерживающей и лишенной какой-либо критики и обвинений «обстановке заботы». Такие нарративы, по предположению авторов, будут способствовать преодолению возможной изоляции членов коллектива и созданию духа профессионального сотрудничества, укрепляющего приверженность организации на основе как заботы о своих пациентах, так и заботы о работающем персонале.
Примечательной чертой исследований 2000–2010‑х гг. также стало подозрительное, а подчас — негативное отношение к такому понятию, как «лояльность организации», в ключе его противопоставления организационной приверженности и удовлетворенности работой.
M. McAllister и L. Stockhausen (2001) [173] замечали, что если приверженность подразумевает «поощрение участия» медсестер в деятельности организации, направленное на своевременное выявление и проблематизацию тех аспектов, которые способны принести ей вред, то лояльность, нередко пропагандируемая и поддерживаемая менеджерами здравоохранения, напротив, ведет к росту ограничений, сдерживанию критики и расцвету конформистских настроений в медсестринских коллективах. К тому же приоритетность влияния врачей на политику больниц ведет к «ощущаемой конкуренции, борьбе за лидерство и путанице в отношении ролей, препятствующей сотрудничеству между практикующими медсестрами и врачами» [174], а высокая степень лояльности руководству провоцирует феномен «группового молчания», когда медсестры из опасений испортить хорошие отношения с руководством предпочитают не сообщать о случаях нарушений, в том числе в части применения небезопасных практик в уходе за пациентами [175].
При этом исследователи подчеркивали, что само наличие доверия к руководителям со стороны персонала вовсе не подразумевает высокой приверженности организации и поддержанию намерений в ней оставаться [176] и, более того, чрезмерная преданность руководству мало влияет на снижение негатива — «уровня цинизма» — по отношению к медицинской организации и «убеждениям относительно ее целостности» [177], но при этом способна спровоцировать более высокие уровни тревожности и депрессии [178][179], а также усиление организационного надзора и контроля качества работы медсестер, что неизбежно вызовет у них разочарование, беспокойство, стрессы, психологические расстройства, семейные проблемы, меньшую организационную приверженность и большее намерение из нее уйти [180]. Неслучайно J. A. Cogin et al. (2016) [181] подмечали, что, когда больницы вводили множество формальных правил, контролирующих установленные процедуры и алгоритмы их выполнения работниками, это приводило к снижению мотивации и негативному отношению к работе, подрывало моральный дух и вызывало разочарование среди медицинских работников.
В связи с этим M. A. Bastos (2001) [182] подчеркивал, что «процесс социализации медсестер», выдержанный в духе лояльности организации, в любом случае будет «пронизан чувствами неуверенности, тревоги, дистресса, некомпетентности и страха», ведущими к разрыву профессиональной карьеры, а J. Rapps et al. (2001) [183] утверждали, что всякая медицинская организация, заинтересованная в укреплении своего кадрового потенциала, должна избавиться от попыток внедрения лояльности и помочь своим сотрудникам стать «самоопределяющимися, независимыми мыслителями», вбирающими в себя необходимые знания, навыки и склонности к критическому мышлению, опыт работы, на основе которых и сформируется организационная приверженность. При этом, по мнению C. Robinson-Walker (2002) [184], для получения устойчивых и высококачественных результатов по формированию организационной приверженности, повышения личной и профессиональной удовлетворенности работой необходимо внедрение не духа лояльности, а коучинга — целенаправленного раскрытия потенциала каждого работника для достижения его жизненных или профессиональных целей с позиций успеха организации.
Еще одной новой особенностью исследований 2000–2010‑х гг. стало заметное расширение их географии: если раньше в подавляющем большинстве случаев изучения организационной приверженности речь шла об опыте европейских или североамериканских больниц (сюда же можно отнести австралийские и новозеландские больницы), то теперь возросло число публикаций, основанных на материалах деятельности азиатских (Китай, Южная Корея, Индия, Саудовская Аравия, Филиппины, Таиланд, Иран, Тайвань, Иордания, Бангладеш), латиноамериканских (Бразилия, Аргентина), а также африканских (Нигерия, Малави, ЮАР, Гана, Эфиопия) медицинских организаций.
Неизбежными следствиями «расширения географии» стало обсуждение вопросов применимости «западного опыта» в условиях других этнокультурных общностей и изучение иных особенностей организационной приверженности в разных уголках планеты — то есть там, где «социальный контекст рынка труда принципиально иной» [185], где ярко представлены различия между коллективистскими и индивидуалистическими культурными взглядами [186], и, наконец, где ситуация зачастую отличается своей политической нестабильностью [187]. Неслучайно S. R. Liou et al. (2013) [188] отмечали, что при анализе приверженности в странах за пределами «золотого миллиарда» следует «использовать культурно обоснованные инструменты, учитывающие культурный контекст, включающий в себя языки и ценности».
Например, характерной чертой исследований китайских авторов (как из КНР, так и из Китайской республики на Тайване) стало обращение внимания на влияние семейных и личностных связей и ценностей на приверженность медсестер. Так, K. Y. Lu et al. (2001) [189] утверждали, что, наряду с уровнем образования и занимаемой должностью, а также статусом больницы, на приверженность активно воздействуют такие факторы, как поддержка семьи, семейное положение и наличие в семье маленьких детей, в частности, заставляющее медсестер-матерей проявлять больше заботы о своих пациентах; F. J. Shih et al. (2002) [190] отмечали, что на укрепление приверженности медицинской организации и в целом профессии влияют: 1) «осознание бренности жизни и желание прожить более значимую жизнь», ценностно связанные с уходом за больными людьми; 2) «забота о ближних и любовь к Родине»; 3) «четкое представление об уходе и лучшее понимание ценности сестринского дела и собственной самооценки»; 4) «глубокое понимание человеческой боли»; и др.
Южнокорейские исследователи W. Y. Park и S. H. Yoon (2009) [191] указывали на то, что ведущую роль в формировании приверженности в «азиатском» духе, росте удовлетворенности работой и отсутствии намерений уйти из организации играют особые представления о справедливости: «процедурной» (связывающей медсестру и ее пациента), «распределительной» (формирующей безусловную преданность руководителям больницы) и «справедливости взаимодействия» (сплачивающей медсестринский коллектив в единое целое).
Индийские исследователи W. L. Cheah et al. (2012) [192] акцентировали внимание на том, что в основе организационной приверженности вообще лежит «общее восприятие управления системой охраны труда» медсестер, предлагая каждой больнице назначить лидеров, обладающих соответствующими навыками руководства и надзора и приверженных обучению персонала.
Иранские исследователи R. Memarian et al. (2008) [193] указывали на то, что главную роль в формировании организационной приверженности играет руководитель больницы как ее «духовный лидер», являющийся образцом нравственного поведения и «духовным наставником для медсестер», наделяющий их соответствующей «духовной силой» и дающий видение четких и ясных целей сестринского дела. A. Ravari et al. (2013) [194] подчеркивали, что приверженность базируется на «духовном удовольствии и удовлетворении» медработников, считающих сестринское дело «божественной профессией и инструментом», основанным на ценностях «внутренней гармонии», «традиционной приверженности» и «духовного единства». A. N. Nasrabadi et al. (2016) [195] видели в основе организационной приверженности альтруизм, включающий в себя защиту интересов пациента, духовную удовлетворенность работой и профессиональную приверженность; при этом «удовлетворенность работой, возникающая в результате альтруизма, воспринимается как приятное чувство вместе с удовольствием, возникающим в результате удовлетворения потребностей пациента, который с нетерпением ждет защиты со стороны медсестры».
Бразильские исследователи M. A. Trevizan et al. (2008) [196] при изучении вопросов организационной приверженности среднего медперсонала выводили на первый план проблемы переосмысления поведенческой приверженности, основанной на рисках, неопределенности, духовной и этической вовлеченности, честности и связанной с различными «измерениями Бытия»; в целом же, по мнению авторов, стимулирование критического осмысления медсестрами проблем гуманности человеческого капитала организаций должно стать неотъемлемой ценностью в процессах управления сестринским делом.
Не следует при этом думать, что «западным» авторам присуща исключительно прагматичность и некая «бездуховность» в их рассуждениях по проблемам организационной приверженности: например, B. Pesut et al. (2009) [197] отмечали, что «духовность» занимает особое место в профессиональной жизни медсестры, подтверждая 3 незыблемые истины: 1) «Все люди духовны»; 2) «Человеческую духовность можно оценить и измерить»; 3) «Духовность является надлежащей областью заботы и вмешательства медсестры». С другой стороны, духовность может оказаться «разменной монетой» для противопоставления людей разных культур и взглядов, свидетельством чему может служить очень спорное исследование I. Kagan et al. (2017) [198], в рамках которого авторы безапелляционно заявляли, что «патриотизм имеет религиозные и культурные измерения. Культурные различия объясняют разницу в организационной приверженности между медсестрами, родившимися в Израиле, и иммигрантами».
Африканские исследователи, в свою очередь, подчеркивали, что в странах с громадным количеством разных языков и межплеменными контрастами приверженность среднего медперсонала зависит в первую очередь от его способности к коммуникации с представителями разных культур [199], а попытки «тонко настроить» систему организационных обязательств на «западный манер» требуют большей гибкости «в соответствии с национальными (здравоохранительными) целями» [200]. Кроме этого, средним медработникам, как и врачам, приходится не только заниматься решением своих непосредственных задач, связанных с организацией ухода за больными людьми, но в целом выступать «защитниками в области прав человека» [201], нередко при этом рискуя своей жизнью и здоровьем.
Впрочем, вопросы приверженности мало волнуют африканских исследователей, так как «головной болью» большинства их стран (особенно к югу от Сахары) оказывалась либо глобальная нехватка кадров, для преодоления которой не существует «волшебного решения» [202], либо катастрофически низкая заработная плата и отсутствие на местах «наборов внутренних правил и руководства с хорошими управленческими качествами» [203]. В этой связи авторы публикаций подчеркивали, что в большей степени актуальна не приверженность африканских медсестер организации, а, учитывая масштабы «утечки мозгов» в более развитые страны, их приверженность работе в своей стране в целом [204].
Надо заметить, что во второй половине 2010‑х гг. тема организационной приверженности казалась в достаточной степени исчерпанной; статей, посвященных данной проблематике, стало заметно меньше, а публикации исследователей в основном вращались вокруг «триады» взаимодействий организационной приверженности (в первую очередь аффективной), «межличностной» справедливости (или профессионального призвания) и намерения текучести кадров.
4. Интегративный, междисциплинарный этап — с начала 2020‑х гг.
Новый поворот в исследовательских поисках наблюдался на рубеже 2010/2020‑х гг. и отразил те глобальные перемены в мировом здравоохранении и организации сестринской деятельности, которые произошли под влиянием пандемии новой коронавирусной инфекции (НКВИ, COVID-19), когда «медицинские работники продемонстрировали сильный коллективистский дух и чувство солидарности, что помогло им справиться с дополнительным стрессом и рабочей нагрузкой» [205].
В частности, обсуждение проблем организационной приверженности стало в большей мере фокусироваться на вопросах сохранения кадрового потенциала в целом в условиях как вынужденного (по причине сокращения штатов), так и добровольного ухода среднего медицинского персонала не только из организаций, но и из профессии. Описывая ситуацию, H. J. Langster и S. Cutrer (2021) [206] эмоционально восклицали: «Деморализация выживших и потеря доверия к организации являются основными результатами… Эти глубокие эмоциональные реакции на нарушение психологического контракта приводят к снижению организационного гражданского поведения, организационной приверженности, производительности и желания сотрудников работать».
Более того, в новых условиях, по мнению исследователей, на первый план вышли проблемы нейтрализации психосоциальных рисков, влияющих на психофизиологическое здоровье работников из-за воздействия длительного стресса, порождающего синдром выгорания и влекущего за собой отток специалистов [207], когда и приверженность профессии, и приверженность организации зависит от воспринимаемого «чувства безопасности» на работе, связанного не только и не столько с усталостью, сколько с присутствием угроз как здоровью, так и жизни медсестер [208]. Неслучайно J. Jun et al. (2021) [209] подчеркивали, что проблема эмоционального и профессионального выгорания обрела теперь не индивидуальный, а коллективный характер, затрагивая в комплексе весь спектр пребывания медсестры в больнице, а именно безопасность и удовлетворенность пациентов, качество ухода, организационную приверженность и производительность, а A. D. G. Atalla et al. (2025) [210] отмечали, что налицо кризис организационной приверженности, проявляющий себя, в частности, в «болезненном презентеизме» — ситуации, когда работник проводит на рабочем месте больше времени, чем это необходимо, но в силу плохого самочувствия работает менее эффективно.
Именно поэтому, по мнению M. Rodríguez-Fernández et al. (2021) [211], возникла потребность в разработке новых моделей организационной приверженности, направленных как на повышение производительности труда, так и на обеспечение «качества здоровья», с формированием соответствующей политики управления медицинскими организациями, ориентированной на поиск приверженности и удовлетворенности работой, так как «важно разрабатывать инновационные практики, связанные с четким дизайном работы и устраняющие причины неопределенности и стресса». Для разработки и внедрения таких практик необходимо «создать позитивный климат, предоставив медсестрам возможности для повышения их компетентности, связанности и автономии посредством активного участия» [212].
Важную роль неформальных лидеров, заботящихся как о профессиональном росте и адаптации молодых сотрудников, так и об укреплении кадрового потенциала медицинских организаций в новых условиях, по мнению ряда исследователей, должны играть, с одной стороны, наставники («наставнические отношения способствуют карьерному оптимизму подопечных, усиливая их организационную приверженность. Больницы должны предоставлять медсестрам пространство для проявления их способностей, расширять возможности для улучшения их способности к командному сотрудничеству, четко определять объем работы и права медсестер и предоставлять медсестрам право принимать решения» [213]), с другой — профессиональные сестринские организации, способствующие продвижению этики и ценностей профессии, «содействующие внедрению организационных инноваций, отстаивающие права медсестер, социальную справедливость и доверие общества» [214].
Не менее важным также является то, на рубеже 2010/2020‑х гг. исследователи обратились к анализу проблем, вызванных трансформационными изменениями в системе оказания медицинской помощи и в работе организаций здравоохранения и связанных, с одной стороны, с процессами цифровизации и расширением применения искусственного интеллекта (например, через призму модели ChatGPT), а с другой — с ростом мультикультурности самих медсестринских коллективов.
К примеру, I. Gibson et al. (2024) [215] отмечали, что понимание факторов, влияющих на внедрение цифровых инструментов в клиническую практику, само по себе представляет очень важную и перспективную область научных исследований, ориентированных на комплексное понимание проблем взаимодействия и взаимовлияния как внутренней среды медицинской организации — приверженности и мотивации работников, поддержки руководства, рабочей нагрузки, воспринимаемого соответствия своей рабочей роли, особенностей организационной культуры и командной работы, так и ее внешней среды — технических и кадровых возможностей, цифровых платформ, инструментов самоконтроля пациентов, цифровой инфраструктуры и пр.
По поводу последствий цифровизации в ключе ее влияния на формирование и поддержание организационной приверженности среднего медперсонала мнения исследователей расходятся.
С одной стороны, D. Sommer et al. (2024) [216] указывают на то, что цифровизация за счет сокращения документации и увеличения времени для обслуживания пациента способна позитивно воздействовать на рост удовлетворенности условиями труда и повышение возможностей карьерного роста, что сможет «привязать» медсестер к своей организации и препятствовать желанию ее покинуть; D. Adam et al. (2023) [217] отмечают, что использование цифровых приложений, включающих в себя адаптированные программы снижения стресса на основе осознанности в сочетании с аспектами поведенческой терапии, когнитивно-поведенческой терапии или терапии принятия и приверженности, в перспективе могут быть внедрены в практику работы с медицинскими работниками и способствовать снижению воздействия психосоциальных рисков на поддержание их желания оставаться в своей организации.
С другой стороны, C. A. Mather et al. (2018) [218], напротив, призывают проявлять максимальную осторожность при внедрении цифровых технологий в практику оказания медицинской помощи пациентам, так как, несмотря на растущее понимание преимуществ, связанных с их использованием, представители сестринского дела «не хотят проявлять активность и бросать вызов традиционным моделям работы, чтобы изменить статус-кво», а A. L. Watson (2024) [219] — не навязывать сверху цифровые технологии и не пытаться приказывать медсестрам, что им надлежит делать, так как последние должны сами отыскать «тонкий баланс между искусственным интеллектом и основными ценностями эмпатии и сострадания… в сочетании с непоколебимой этической приверженностью».
Вторая, не менее важная тема, обратившая на себя внимание в 2020‑е гг., связана с ростом мультикультурности коллективов среднего медицинского персонала и возникающих в связи с этим вопросов поддержания и укрепления его связей со своими организациями. По мнению H. G. Jeon et al. (2024) [220], «ориентация на чувствительность к разнообразию и позитивная организационная культура сестринского дела оказывают двойной посреднический эффект на связь между управлением разнообразием и организационной приверженностью», а V. Morrison et al. (2021) [221] подчеркивают, что разнообразие, равенство и инклюзивность в сестринском деле сами по себе способствуют как укреплению организационной приверженности, так и «расширению структурных прав и возможностей в направлении более разнообразной, справедливой и инклюзивной организации».
Актуальной отсюда становится проблема конструирования «культуры воспринимаемой справедливости» как «краеугольного камня» любой организации, стремящейся обеспечить безопасность, создать систему обратной связи с сотрудниками и совершенствовать их организационную идентификацию и заинтересованность в процветании их учреждения здравоохранения [222]. При этом, как утверждают A. Ito et al. (2023) [223], аффективная приверженность медсестры, с одной стороны, положительно связана с процедурной справедливостью (справедливостью вознаграждений) и интеракционной справедливостью (справедливостью взаимодействий, основанных на уважительном отношении к работнику), существующих в отдельных подразделениях медицинских организаций, но с другой — опосредуется работником на уровне личностного восприятия («индивидуальной справедливости»). В целом же, как полагают J. Buss и D. Arnold (2023) [224], необходимо избавиться от диссонанса, возникающего между профессиональными ценностями медсестер и неолиберальными ценностями, воплощенными в системе здравоохранения, и нередко приводящего к потере способностей жить в соответствии со своими моральными идеалами и отстаивать социальную справедливость.
ОБСУЖДЕНИЕ
Суммируя опыт измерения уровня организационной приверженности среднего медицинского персонала и разработки конкретных мероприятий по его повышению, A. G. Lee и K. D. Carter (2004) [225] справедливо замечают, что, подобно измерению результатов процессов обучения, основные проблемы заключаются в поисках конкретных инструментов и критериев оценивания. Как утверждают исследователи, к последним в первую очередь может быть отнесено наличие нескольких оценок разных наблюдателей с использованием разных инструментов в разные периоды времени; при этом сами «инструменты» должны быть надежными, воспроизводимыми, действительными и практичными, то есть осуществимыми, удобными, требующими небольших временных затрат, простыми в использовании и недорогими для внедрения и обслуживания; они должны представлять собой не просто констатацию фактов на основе полученных качественных и/или количественных данных, но быть ориентированными на улучшения в будущем. Сам же процесс оценивания должен быть справедливым, объективным и связан с реальной действительностью, а шкала оценок должна быть открытой и четко определенной.
Неслучайно S. O. Choi (2005) [226] замечает, что конструирование модели приверженности медицинской организации требует огромных усилий, так как приверженность должна учитывать органическую взаимосвязь удовлетворенности работой, производительности труда, намерений покинуть рабочее место, способностей работника принимать самостоятельные решения и общих результатов организационной социализации, с одной стороны, и организационных и индивидуальных ценностей, знаний и навыков, связанных с выполнением задач, эмоций и особенностей коммуникации медицинских сестер, с другой стороны, а также конструктивного учета того, чего хотят сами медработники с позиций получения ими личных (возможно, «корыстных») результатов [227].
В этой связи исследователи призывают обращать внимание на «качество трудовой жизни» медсестер, выражающее смысл организационной приверженности и являющееся интегральной «системой анализа того, как они воспринимают работу, как она связана с удовлетворенностью работой, намерением уйти, текучестью кадров, личностью и стрессом на работе» [228], в связи с чем B. M. Schrems (2013) [229] указывала, что необходимо заполнить пробелы в области сестринского дела с ориентацией исследователей на изучение «процессов, сообщества, контекста и отношений», а A. Hofmeyer и P. B. Marck (2008) [230] замечали, что руководителям следует использовать ресурсы «социального капитала» медсестер, предпринимая конкретные шаги по выделению необходимых человеческих и материальных ресурсов для: 1) налаживания отношений по «укреплению связей и наведению мостов»; 2) укрепления солидарности и доверия; 3) содействия коллективным действиям и сотрудничеству; 4) укрепления коммуникации и поощрения обмена знаниями; 5) создания потенциала для социальной сплоченности и инклюзивности.
ЗАКЛЮЧЕНИЕ
На основе анализа научных публикаций, обращенных к изучению вопросов приверженности среднего медицинского персонала своим организациям, авторами выделены 4 хронологических этапа.
Итак, на первом, начальном, этапе (рубеж 1960/1970‑х — 1980‑е гг.) публикации еще очень редки и, как правило, носят описательный характер, касающийся обязательств среднего медперсонала, его приверженности этическим моделям поведения и роли ценностей профессии. В то же время появляются статьи, содержащие призывы к разработке «систем объективных оценок программ охраны труда» среднего медперсонала, учитывающих разнообразные аспекты «трудовой жизни», а также влияние «ролевой неопределенности» и «ролевых конфликтов» на желание длительное время работать в медицинской организации.
Второй этап (1990‑е гг.) характеризуется активизацией научных поисков, связанных со стремлением исследователей понять настроения среднего медперсонала в ключе разработки и применения методик изучения вовлеченности и удовлетворенности трудом, в частности того, что лежит в основе и определяет приверженность к длительной работе в медицинской организации. В этой связи появляются публикации, обращенные к анализу особенностей «личного жизненного опыта», проблем внедрения психологических контрактов, конструирования моделей «совместного управления», создания «самостоятельных рабочих групп медсестер» («сообществ на рабочем месте») и «совместных команд» и пр.; отмечается необходимость вовлечения медсестер в управление организациями и установления на местах «баланса сил», обеспечивающего права среднего медперсонала. Тем самым этап изучения вовлеченности и удовлетворенности акцентирует внимание на личном опыте, внедрении психологических контрактов, совместном управлении и рабочих группах.
Третий этап (рубеж 1990/2000‑х — начало 2020‑х гг.) ознаменовался широким «внедрением социологии» в исследовательскую практику: появляется множество публикаций, посвященных измерению уровней аффективной, инерционной и нормативной приверженности среднего медперсонала на основе применения модели Дж. Мейера и Н. Аллен. В то же время большое значение обретает анализ «особости» медсестринского труда; в частности, авторы обращают внимание на необходимость формирования «культуры учреждений», нахождения «точек соприкосновения» с ожиданиями сотрудников, создания атмосферы воспринимаемой поддержки в виде неформальных социальных сетей и эффективных сетей коммуникации. В поле зрения исследователей оказались вопросы эмоциональных составляющих труда среднего медперсонала и их влияния на приверженность организации с анализом таких аспектов, как эмоциональное истощение, стрессы и стрессоры, профессиональное выгорание, деперсонализация и пр. Наконец, наблюдается процесс расширения географии исследований, совмещенный с попытками понять специфику организационной приверженности за пределами «западного опыта». В целом же этап измерения и анализа эмоциональных аспектов акцентировал внимание на развитии моделей оценки приверженности, исследовании особенностей сестринского труда и эмоционального выгорания.
Четвертый этап (с начала 2020‑х гг.), спровоцированный событиями пандемии НКВИ, обнаруживает значительно возросшее внимание исследователей к вопросам безопасности персонала на рабочих местах, коллективного эмоционального и профессионального выгорания и в целом сохранения «качества здоровья» среднего медперсонала. Показательным становится появление новых тем, связанных с изучением влияния цифровизации и мультикультурности на поддержание организационной приверженности и стабильности медсестринских коллективов.
В целом в дискуссиях по вопросам содержания организационной приверженности среднего медицинского персонала и проблемам его качественного измерения рано ставить точку, так как реальная жизнь ставит все новые и новые проблемы, требующие адекватного изучения и детального научного анализа.
Таблица. Этапы изучения организационной приверженности среднего медицинского персонала
Table. Stages of studying organizational commitment among nursing staff
|
Этап |
Содержание исследований |
Цели исследований и направленность публикаций |
Результаты и академические выводы |
|
1. Начальный этап формирования концепции: конец 1960‑х — начало 1990‑х гг. |
Определение и первичное осмысление понятия |
Установление базовых определений и концептов приверженности в профессии медицинской сестры и организации |
Установлена значимость организационной приверженности как психологического феномена для устойчивости персонала в организациях |
|
2. Классический этап моделирования концепции: 1990‑е гг. |
Разработка теоретических моделей и систематизация |
Разработка теоретических моделей, изучение факторов и последствий организационной приверженности |
Теоретическое осмысление трехкомпонентной модели приверженности; расширено понимание механизмов формирования |
|
3. Прикладной этап «внедрения социологии»: рубеж 1990/2000‑х — начало 2020‑х гг. |
Эмпирические исследования влияния на качество услуг |
Оценка влияния приверженности на рабочие процессы, качество медицинской помощи и кадровую устойчивость |
Подтверждена связь организационной приверженности с повышением качества услуг и снижением текучести кадров |
|
4. Интегративный, междисциплинарный этап: с начала 2020‑х гг. |
Междисциплинарный анализ, расширение методов |
Интеграция различных подходов, применение сложных методик, практическое применение |
Выявлена мультикомпонентная природа приверженности, расширены методы измерения, усилена ориентация на практические решения в управлении здравоохранением |
Примечание: таблица составлена авторами.
Note: The table was compiled by the authors.
ТЕОРЕТИЧЕСКАЯ И ПРАКТИЧЕСКАЯ ЗНАЧИМОСТЬ
Теоретическая значимость исследования заключается в систематизации и углублении понимания организационной приверженности, что расширяет теоретическую базу и способствует развитию концептуальных моделей. Практическая значимость — в обосновании использования организационной приверженности как инструмента для повышения эффективности управления персоналом в здравоохранении и решения актуальных кадровых проблем. Это позволяет разрабатывать адресные стратегии мотивации и удержания медицинских специалистов, улучшая качество медицинских услуг и стабильность кадровых ресурсов.
Результаты обзора могут стать основой для разработки новых инструментов оценки и программ повышения организационной приверженности среднего медперсонала в российских медицинских организациях по следующим направлениям:
- Адаптация зарубежных моделей оценки. Использование валидированных зарубежных инструментов (например, модели Дж. Мейера и Н. Аллен) с учетом российских реалий позволит создавать надежные и воспроизводимые методики измерения приверженности, которые отражают не только удовлетворенность трудом, но и ценностные ориентации, профессиональную идентичность, восприятие поддержки и безопасность труда.
- Разработка объективных и простых в применении шкал. В обзоре подчеркивается необходимость создания инструментов, которые будут простыми, малозатратными, справедливыми и максимально приближенными к реальной практике, что важно для их массового внедрения в организациях здравоохранения.
- Ориентация на организационные улучшения. Полученные с помощью новых инструментов данные должны использоваться не только для констатации уровня приверженности, но и для целенаправленного совершенствования организационной культуры, повышения вовлеченности, профилактики выгорания и формирования атмосферы поддержки персонала.
- Учет современных вызовов. Программы повышения приверженности должны включать компоненты, связанные с цифровизацией, мультикультурностью, коллективной безопасностью и профилактикой эмоционального выгорания, что отражает современные тенденции в зарубежных исследованиях и актуально для российских условий.
- Вовлечение персонала в управление. Важным направлением является внедрение практик совместного управления, формирования самостоятельных рабочих групп и психологических контрактов, что способствует росту вовлеченности и ответственности среднего медперсонала.
1. Указ Президента РФ от 07.05.2024 г. № 309 «О национальных целях развития Российской Федерации на период до 2030 года и на перспективу до 2036 года». Available: http://kremlin.ru/events/president/news/73986 (дата обращения: 28.09.2025).
2. Дата обращения — 27.03.2025 г.
3. Партисипативное управление — управление, направленное на раскрепощение творческой активности работников и обеспечивающее их вовлечение в управление организацией.
4. Фасилитирующее лидерство — умение формального или неформального лидера организовать процесс командной работы с максимальным использованием потенциала сотрудников.
5. Подобная ситуация сохранится и в дальнейшем — в более поздних публикациях.
Список литературы
1. Алексеева Е.А. Концепт организационной приверженности в социологической дискуссии. Казанский социально‑гуманитарный вестник. 2022;6(57):4–10. https://doi.org/10.26907/2079-5912.2022.6.4-10
2. Липатов С.А. Проблема взаимодействия человека и организации: концепции и направления исследований. Вестник Московского университета. Серия 14. Психология. 2012;1:85–96.
3. Липатов С.А., Синчук Х.И. Социально-психологические факторы организационной приверженности сотрудников (на примере коммерческих организаций). Организационная психология. 2012;5(4):6–28.
4. Ловаков А.В., Липатов С.А. Организационная идентификация и приверженность персонала: сходство и различие. Психология. Журнал Высшей школы экономики. 2011;8(2):69–80.
5. Ранова Л.Н. Управление человеческими ресурсами: особенности людей, мотивация, приверженность, организационная культура. Вестник магистратуры. 2014; 2(3(30));18–20.
6. Трофимова Е.Л., Бондаренко В.Ю. Проблема приверженности персонала к организации в отечественной и зарубежной литературе. Психология в экономике и управлении. 2013;1:28–36.
7. Чернякевич Е.Ю. Лидерский потенциал и карьерные ориентации как предикторы организационной приверженности молодых специалистов: гендерный аспект. Известия Иркутского государственного университета. Серия Психология. 2023;44:85–98. http://dx.doi.org/10.26516/2304-1226.2023.44.85
8. Потапова Ю.В., Климухина В.А. Структура и факторы формирования организационной приверженности: теоретическая модель. Организационная психология. 2024;14(3):117–146. https://doi.org/10.17323/2312-5942-2024-14-3-117-146
9. Meyer JP, Allen NJ. A three-component conceptualization of organizational commitment. Human Resource Management Review. 1991;1(1):61–89. http://dx.doi.org/10.1016/1053-4822(91)90011-z
10. Умнов С.В., Берсенева Е.А., Кудрина В.Г., Андреева Т.В., Спасенников Б.А. Современные подходы к формированию высокой приверженности персонала медицинской организации. Бюллетень Национального научно‑исследовательского института общественного здоровья имени Н.А. Семашко. 2022;1–2:42–49. https://doi.org/10.25742/NRIPH.2022.01.005
11. 1967: a time for commitment. Ohio Nurses Rev. 1967;42(1):7–12.
12. Notter LE. The profession’s commitment. N Y State Nurse. 1967;39(2):6–10.
13. Henderson V. Some commitments for nurses today. Alumnae Mag Columbia Univ Presbyt Hosp Sch Nurs Alumnae Assoc. 1968;63(1):5–15.
14. Mullane MK. Today’s challenges--tomorrow’s commitments. Va Nurse Q. 1977;45(4):6–10.
15. Schlotfeldt RM. Nursing research: reflection of values. Nurs Res. 1977;26(1):4–9.
16. Recommendations spell out commitment. RNABC News. 1979;11(5):22–23.
17. Smith JP. The challenge of health education for nurses in the 1980s. J Adv Nurs. 1979;4(5):531–543. https://doi.org/10.1111/j.1365-2648.1979.tb00886.x
18. Nichols B. Belonging to your professional organization: a commitment to personal growth and professional development. Imprint. 1980;27(4):18.
19. Holland D. A grass roots approach to developing inpatient nursing unit work groups. J Neurosurg Nurs. 1984;16(4):217–220. https://doi.org/10.1097/01376517-198408000-00009
20. Hicks F. Nursing: health care’s best resource--fulfilling the commitment. Oreg Nurse. 1986;51(2):12–15.
21. Zander K. Nursing case management. Resolving the DRG paradox. Nurs Clin North Am. 1988;23(3):503–520.
22. Patterson DL. Achieving excellence in nursing. J Pediatr Nurs. 1991;6(6):391–395.
23. Krause K. Sairaanhoitajan ammatin kehittämisestä [Development of the nursing profession]. Sairaanhoitaja (1991). 1993;(4):25–27. Finnish.
24. Martin PJ. One meter stick--the nursing audit. J Adv Nurs. 1980;5(2):199–208. https://doi.org/10.1111/j.1365-2648.1980.tb00950.x
25. Melia KM. Student nurses’ construction of occupational socialisation. Sociol Health Illn. 1984;6(2):132–151. https://doi.org/10.1111/1467-9566.ep10778231
26. Barbiasz JE, Hunt V, Lowenstein A. Nursing documentation: a format not a form. J Nurs Adm. 1981;11(6):22–26.
27. Ouellet D, Elsner C. A roadmap for the novice researcher. Can J Cardiovasc Nurs. 1993;4(2):16–19.
28. Corley MC, Mauksch HO. The nurse’s multiple commitments. J Prof Nurs. 1993;9(2):116–122. https://doi.org/10.1016/8755-7223(93)90028-b
29. Ring N. A personal and historical investigation of the career trends of UK graduate nurses qualifying between 1970 and 1989. J Adv Nurs. 2002;40(2):199–209. https://doi.org/10.1046/j.1365-2648.2002.02362.x
30. Webb SB Jr. Objective criteria for evaluating occupational health programs. Am J Public Health. 1975;65(1):31–37. https://doi.org/10.2105/ajph.65.1.31
31. Britton L. Use of behavioral science concepts and processes to facilitate change: a team building program for nursing supervisors. Aust Health Rev. 1984;7(3):162–179.
32. Morison MJ. Promoting the motivation to change. The role of facilitative leadership in quality assurance. Prof Nurse. 1992;7(11):715–716, 718.
33. Stichler JF. Shared governance: what it means to those involved. Aspens Advis Nurse Exec. 1989;4(9):1, 3, 6–8.
34. Coyne C, Killien M. A system for unit-based monitors of quality of nursing care. J Nurs Adm. 1987;17(1):26–32.
35. Porter-O’Grady T. Shared governance for nursing. Part II: Putting the organization into action. AORN J. 1991;53(3):694–703. https://doi.org/10.1016/s0001-2092(07)68943-1
36. Doherty C, Hope W. Shared governance--nurses making a difference. J Nurs Manag. 2000;8(2):77–81. https://doi.org/10.1046/j.1365-2834.2000.00162.x
37. Smith HL. Nurses’ quality of working life in an HMO: a comparative study. Nurs Res. 1981;30(1):54–58. https://doi.org/10.1097/00006199-198101000-00018
38. Rosse JG, Rosse PH. Role conflict and ambiguity: an empirical investigation of nursing personnel. Eval Health Prof. 1981;4(4):385–405. https://doi.org/10.1177/016327878100400403
39. Jamal M. Job stress and job performance controversy: an empirical assessment. Organ Behav Hum Perform. 1984;33(1):1–21. https://doi.org/10.1016/0030-5073(84)90009-6
40. McCloskey JC. Two requirements for job contentment: autonomy and social integration. Image J Nurs Sch. 1990;22(3):140–143. https://doi.org/10.1111/j.1547-5069.1990.tb00196.x
41. Kraemer LG, Rigolizzo-Gurenlian J. Role conflicts in nursing and allied health: a comparison of professional and organizational commitment. J Allied Health. 1985;14(1):53–62.
42. Christensen PJ. An ethical framework for nursing service administration. ANS Adv Nurs Sci. 1988;10(3):46–55. https://doi.org/10.1097/00012272-198804000-00006
43. Moran MJ, Johnson JE. Quality improvement: the nurse’s role. ANA Publ. 1992;(NP-80 7.5 M):45–61.
44. Bousfield C. A phenomenological investigation into the role of the clinical nurse specialist. J Adv Nurs. 1997;25(2):245–256. https://doi.org/10.1046/j.1365-2648.1997.1997025245.x
45. Mulholland J. Assimilating sociology: critical reflections on the ‘sociology in nursing’ debate. J Adv Nurs. 1997;25(4):844–852. https://doi.org/10.1046/j.1365-2648.1997.1997025844.x
46. Blegen MA. Nurses’ job satisfaction: a meta-analysis of related variables. Nurs Res. 1993;42(1):36–41.
47. Acorn S, Ratner PA, Crawford M. Decentralization as a determinant of autonomy, job satisfaction, and organizational commitment among nurse managers. Nurs Res. 1997;46(1):52–58. https://doi.org/10.1097/00006199-199701000-00009
48. Davies SM. An evaluation of nurse-led team care within a rehabilitation ward for elderly people. J Clin Nurs. 1994;3(1):25–33. https://doi.org/10.1111/j.1365-2702.1994.tb00355.x
49. McNeese-Smith DK. The influence of manager behavior on nurses’ job satisfaction, productivity, and commitment. J Nurs Adm. 1997;27(9):47–55. https://doi.org/10.1097/00005110-199709000-00011
50. Knox S, Irving JA. Nurse manager perceptions of healthcare executive behaviors during organizational change. J Nurs Adm. 1997;27(11):33–39. https://doi.org/10.1097/00005110-199711000-00008
51. Salyer J, Geddes N, Smith CS, Mark BA. Commitment and communication: keys to minimizing attrition in multisite longitudinal organizational studies. Nurs Res. 1998;47(2):123–125. https://doi.org/10.1097/00006199-199803000-00012
52. Cavanagh SJ. A ‘new’ psychological contract for nurses: some management implications. J Nurs Manag. 1996;4(2):79–83.
53. Molzahn AE. Creating caring organization cultures in dialysis units. ANNA J. 1997;24(2):247–253.
54. Johansson I, Larsson G, Hamrin E. Changes of nursing organization in a surgical department: effects on work satisfaction and quality of care. J Clin Nurs. 1994;3(3):169–175. https://doi.org/10.1111/j.1365-2702.1994.tb00382.x
55. MacDonald G. Shared governance--a unit based concept. Axone. 1995;17(1):3–5.
56. Narayan MC, Tennant J, Larose P, Grumbly J, Marchessault L. Achieving success in home care through the self-directed work group approach. Home Healthc Nurse. 1996;14(11):865–872; quiz 874–875. https://doi.org/10.1097/00004045-199611000-00004
57. Annand F. The mentor commitment. Insight. 1997;22(2):41–45. https://doi.org/10.1016/s1060-135x(97)90044-0
58. Parker M, Gadbois S. The fragmentation of community: Part 1, The loss of belonging and commitment at work. J Nurs Adm. 2000;30(7–8):386–390. https://doi.org/10.1097/00005110-200007000-00015
59. Wilson CK. Team behaviors: working effectively in teams. Semin Nurse Manag. 1998;6(4):188–194.
60. McCrea MA. Personal reflections on early learning in shared leadership. Semin Nurse Manag. 1998;6(2):83–88.
61. Makaram S. Interprofessional cooperation. Med Educ. 1995;29 Suppl 1:65–69. https://doi.org/10.1111/j.1365-2923.1995.tb02893.x
62. Corrales D, Galindo A, Escobar MA, Palomo L, Magariño MJ. El debate sobre la organización, las funciones y la eficiencia de enfermería en atención primaria: a propósito de un estudio cualitativo [The debate on the organization, functions and efficiency of nursing in primary care: apropos of a qualitative study]. Aten Primaria. 2000;25(4):214–219. Spanish. https://doi.org/10.1016/s0212-6567(00)78489-7
63. Caricati L, Mancini T, Bianconcini M, Guidi C, Prandi C, Silvano R, Sollami A, Tafurelli C, Artioli G. Psychosocial predictors of collaborative practice between nurses and physicians working in hospitals. Acta Biomed. 2014;85(3):32–40.
64. Brewer AM, Lok P. Managerial strategy and nursing commitment in Australian hospitals. J Adv Nurs. 1995;21(4):789–799. https://doi.org/10.1046/j.1365-2648.1995.21040789.x
65. Dwore RB, Murray BP, Fosbinder D, Parsons R, Smith P, Dalley K, Vorderer L, Gustafson G. Integration of nurse executives into executive level administration in Utah hospitals. Health Care Manag (Frederick). 2000;18(4):22–36. https://doi.org/10.1097/00126450-200018040-00005
66. Norsen L, Opladen J, Quinn J. Practice model: collaborative practice. Crit Care Nurs Clin North Am. 1995;7(1):43–52.
67. Cheater FM, Keane M. Nurses’ participation in audit: a regional study. Qual Health Care. 1998;7(1):27–36. https://doi.org/10.1136/qshc.7.1.27
68. Gifford BD, Zammuto RF, Goodman EA. The relationship between hospital unit culture and nurses’ quality of work life. J Healthc Manag. 2002;47(1):13–25; discussion 25–26.
69. Bergler R. Zur Psychologie des Pflegepersonals in der ambulanten Pflege [Psychology of nursing personnel in home care nursing]. Zentralbl Hyg Umweltmed. 1995;197(1–3):45–74. German.
70. Laschinger HK, Havens DS. The effect of workplace empowerment on staff nurses’ occupational mental health and work effectiveness. J Nurs Adm. 1997;27(6):42–50. https://doi.org/10.1097/00005110-199706000-00012
71. Hinds PS, Sanders CB, Srivastava DK, Hickey S, Jayawardene D, Milligan M, Olson MS, Puckett P, Quargnenti A, Randall EA, Tyc V. Testing the stress-response sequence model in paediatric oncology nursing. J Adv Nurs. 1998;28(5):1146–1157. https://doi.org/10.1046/j.1365-2648.1998.00731.x
72. Frederick B, Frederick L. Quality improvement with a culturally diverse staff: implications for nurse managers. Semin Nurse Manag. 1995;3(3):137–142.
73. Cioffi RN. Communicating with culturally and linguistically diverse patients in an acute care setting: nurses’ experiences. Int J Nurs Stud. 2003;40(3):299–306. https://doi.org/10.1016/s0020-7489(02)00089-5
74. Pappas SH. Creating an environment to support hardiness and quality patient care. Semin Nurse Manag. 1995;3(3):115–118.
75. Shaver KH, Lacey LM. Job and career satisfaction among staff nurses: effects of job setting and environment. J Nurs Adm. 2003;33(3):166–172. https://doi.org/10.1097/00005110-200303000-00008
76. Woodward VM. Professional caring: a contradiction in terms? J Adv Nurs. 1997;26(5):999–1004. https://doi.org/10.1046/j.1365-2648.1997.00389.x
77. Modic MB, Amour M. Putting compassion and commitment back into nursing. Aspens Advis Nurse Exec. 1998;13(8):1, 3–6.
78. Farley CL. Service learning: applications in midwifery education. J Midwifery Womens Health. 2003;48(6):444–448. https://doi.org/10.1016/j.jmwh.2003.08.010
79. Salvage J. Evidence-based practice: a mixture of motives? Nurs Times. 1998;94(23):61–64.
80. Hem MH, Heggen K. Is compassion essential to nursing practice? Contemp Nurse. 2004;17(1–2):19–31. https://doi.org/10.5172/conu.17.1-2.19
81. Beagan B, Ells C. Values that matter, barriers that interfere: the struggle of Canadian nurses to enact their values. Can J Nurs Res. 2009;41(1):86–107.
82. Rogut L, Hudson A. Meeting patients’ needs: quality care in a changing environment. Pap Ser United Hosp Fund N Y. 1995:1–33.
83. Westrope RA, Vaughn L, Bott M, Taunton RL. Shared governance. From vision to reality. J Nurs Adm. 1995;25(12):45–54. https://doi.org/10.1097/00005110-199512000-00008
84. Peterson R. Building a mission for quality care. J Neurosci Nurs. 1999;31(6):363–365. doi: 10.1097/01376517-199912000-00007
85. Naughton M, Nolan M. Developing nursing’s future role: a challenge for the millennium: 1. Br J Nurs. 1998;7(16):983–986. https://doi.org/10.12968/bjon.1998.7.16.5614
86. Woods SS, Jensen LB, Schulz P, Barnason S, Graham J, Rasmussen D, Carder B, Wild MC. Collaborative research: a community approach. Clin Nurse Spec. 2000;14(1):13–16. https://doi.org/10.1097/00002800-200001000-00008
87. Kalbfleisch PJ, Bach BW. The language of mentoring in a health care environment. Health Commun. 1998;10(4):373–392. https://doi.org/10.1207/s15327027hc1004_5
88. Cangelosi JD Jr, Markham FS, Bounds WT. Factors related to nurse retention and turnover: an updated study. Health Mark Q. 1998;15(3):25–43. https://doi.org/10.1300/J026v15n03_02
89. Barrett L, Yates P. Oncology/haematology nurses: a study of job satisfaction, burnout, and intention to leave the specialty. Aust Health Rev. 2002;25(3):109–121. https://doi.org/10.1071/ah020109
90. Dyck D, Roithmayr T. Organizational stressors and health. How occupational health nurses can help break the cycle. AAOHN J. 2002;50(5):213–219.
91. Hirsch NJ. In the patient’s best interest--a call to action, a call to balance. Bioethics Forum. 2002;18(1–2):24–29.
92. Fairfield KD. Whose side are you on? Interdependence and its consequences in management of healthcare delivery. J Healthc Manag. 2004;49(1):17–29; discussion 30–31.
93. Simons M. The cycle of caring. Nurs Adm Q. 2004;28(4):280–284. https://doi.org/10.1097/00006216-200410000-00010
94. Lim VK, Yuen EC. Doctors, patients, and perceived job image: an empirical study of stress and nurses in Singapore. J Behav Med. 1998;21(3):269–282. https://doi.org/10.1023/a:1018769000750
95. Koivula M, Paunonen M, Laippala P. Prerequisites for quality improvement in nursing. J Nurs Manag. 1998;6(6):333–342. https://doi.org/10.1046/j.1365-2834.1998.00091.x
96. Jamal M, Baba VV. Job stress and burnout among Canadian managers and nurses: an empirical examination. Can J Public Health. 2000;91(6):454–458. https://doi.org/10.1007/BF03404828
97. Brunges M, Foley-Brinza C. Projects for increasing job satisfaction and creating a healthy work environment. AORN J. 2014;100(6):670–681. https://doi.org/10.1016/j.aorn.2014.01.029
98. McNeese-Smith DK. Job stages of entry, mastery, and disengagement among nurses. J Nurs Adm. 2000;30(3):140–147. https://doi.org/10.1097/00005110-200003000-00006
99. McNeese-Smith DK, van Servellen G. Age, developmental, and job stage influences on nurse outcomes. Outcomes Manag Nurs Pract. 2000;4(2):97–104
100. Ruokolainen M, Mauno S, Cheng T. Are the most dedicated nurses more vulnerable to job insecurity? Age-specific analyses on familyrelated outcomes. J Nurs Manag. 2014;22(8):1042–1053. https://doi.org/10.1111/jonm.12064
101. Hu J, Herrick C, Hodgin KA. Managing the multigenerational nursing team. Health Care Manag (Frederick). 2004;23(4):334–340. https://doi.org/10.1097/00126450-200410000-00008
102. Keepnews DM, Brewer CS, Kovner CT, Shin JH. Generational differences among newly licensed registered nurses. Nurs Outlook. 2010;58(3):155–163. https://doi.org/10.1016/j.outlook.2009.11.001
103. Farr-Wharton R, Brunetto Y, Shacklock K. The impact of intuition and supervisor-nurse relationships on empowerment and affective commitment by generation. J Adv Nurs. 2012;68(6):1391–1401. https://doi.org/10.1111/j.1365-2648.2011.05852.x
104. Hendricks JM, Cope VC. Generational diversity: what nurse managers need to know. J Adv Nurs. 2013;69(3):717–725. https://doi.org/10.1111/j.1365-2648.2012.06079.x
105. McNeese-Smith DK, Crook M. Nursing values and a changing nurse workforce: values, age, and job stages. J Nurs Adm. 2003;33(5):260–270. https://doi.org/10.1097/00005110-200305000-00002
106. SmithBattle L, Diekemper M, Drake MA. Articulating the culture and tradition of community health nursing. Public Health Nurs. 1999;16(3):215–222. https://doi.org/10.1046/j.1525-1446.1999.00215.x
107. Churchill J. Organizational culture in the changing workplace: an employee assistance program perspective. Semin Nurse Manag. 1999;7(1):17–20.
108. Kroposki M, Murdaugh CL, Tavakoli AS, Parsons M. Role clarity, organizational commitment, and job satisfaction during hospital reengineering. Nursingconnections. 1999;12(1):27–34.
109. Omery A, Williams RP. An appraisal of research utilization across the United States. J Nurs Adm. 1999;29(12):50–56. https://doi.org/10.1097/00005110-199912000-00011
110. Beccaria LM, Fávero N. Expectativas de gerentes e assessores de enfermagem quanto ao estilo gerencial do diretor executivo de um hospital de ensino [Expectations of nursing managers and assistants as to the managerial style of an executive director of a teaching hospital]. Rev Lat Am Enfermagem. 2000;8(2):83–90. Portuguese. https://doi.org/10.1590/s0104-11692000000200013
111. MacPhee M. Hospital networking. Comparing the work of nurses with flexible and traditional schedules. J Nurs Adm. 2000;30(4):190–198. https://doi.org/10.1097/00005110-200004000-00010
112. Manias E, Aitken R, Peerson A, Parker J, Wong K. Agency-nursing work: perceptions and experiences of agency nurses. Int J Nurs Stud. 2003;40(3):269–279. https://doi.org/10.1016/s0020-7489(02)00085-8
113. Laschinger HK, Finegan J, Shamian J. The impact of workplace empowerment, organizational trust on staff nurses’ work satisfaction and organizational commitment. Health Care Manage Rev. 2001;26(3):7–23. https://doi.org/10.1097/00004010-200107000-00002
114. Haney L, Amann MC. Cultivating effectiveness in your organization. AAOHN J. 2001;49(8):369–373.
115. Downey M, Parslow S, Smart M. The hidden treasure in nursing leadership: informal leaders. J Nurs Manag. 2011;19(4):517–521. https://doi.org/10.1111/j.1365-2834.2011.01253.x
116. Curtin LL. The impact of market-based ‘reform’ on cultural values in health care. Semin Nurse Manag. 1999;7(4):198–202.
117. Kuokkanen L, Leino-Kilpi H, Katajisto J. Nurse empowerment, jobrelated satisfaction, and organizational commitment. J Nurs Care Qual. 2003;18(3):184–192. https://doi.org/10.1097/00001786-200307000-00004
118. Badr L, Rizk U, Farha R. The divergent opinions of nurses, nurse managers and nurse directors: the case in Lebanon. J Nurs Manag. 2010;18(2):182–193. https://doi.org/10.1111/j.1365-2834.2010.01052.x
119. Motwani J, Klein D, Navitskas S. Striving toward continuous quality improvement: a case study of Saint Mary’s Hospital. Health Care Manag (Frederick). 1999;18(2):33–40. https://doi.org/10.1097/00126450-199912000-00006
120. Hannigan B, Burnard P. Nursing, politics and policy: a response to Clifford. Nurse Educ Today. 2000;20(7):519–523. https://doi.org/10.1054/nedt.2000.0505
121. Caine RM, Lowenstein H. Messages of professional empowerment from the land of Oz. Crit Care Nurse. 2000;20(5):8, 10, 12–13.
122. Wagner SL, Rush MC. Altruistic organizational citizenship behavior: context, disposition, and age. J Soc Psychol. 2000;140(3):379–391. https://doi.org/10.1080/00224540009600478
123. Murrells T, Robinson S, Griffiths P. Job satisfaction trends during nurses’ early career. BMC Nurs. 2008;7:7. https://doi.org/10.1186/1472-6955-7-7
124. Laschinger HK, Finegan J, Shamian J, Casier S. Organizational trust and empowerment in restructured healthcare settings. Effects on staff nurse commitment. J Nurs Adm. 2000;30(9):413–425. https://doi.org/10.1097/00005110-200009000-00008
125. Laschinger HK, Finegan J, Shamian J, Almost J. Testing Karasek’s Demands-Control Model in restructured healthcare settings: effects of job strain on staff nurses’ quality of work life. J Nurs Adm. 2001;31(5):233–243. https://doi.org/10.1097/00005110-200105000-00003
126. Kuokkanen L, Katajisto J. Promoting or impeding empowerment? Nurses’ assessments of their work environment. J Nurs Adm. 2003;33(4):209–215. https://doi.org/10.1097/00005110-200304000-00005
127. McNeese-Smith DK. A nursing shortage: building organizational commitment among nurses. J Healthc Manag. 2001;46(3):173–186; discussion 186–187.
128. Gellatly IR, Cowden TL, Cummings GG. Staff nurse commitment, work relationships, and turnover intentions: a latent profile analysis. Nurs Res. 2014;63(3):170–181. https://doi.org/10.1097/NNR.0000000000000035
129. Hsu CP, Chiang CY, Chang CW, Huang HC, Chen CC. Enhancing the commitment of nurses to the organisation by means of trust and monetary reward. J Nurs Manag. 2015;23(5):567–576. https://doi.org/10.1111/jonm.12180
130. Lu KY, Lin PL, Wu CM, Hsieh YL, Chang YY. The relationships among turnover intentions, professional commitment, and job satisfaction of hospital nurses. J Prof Nurs. 2002;18(4):214–219. https://doi.org/10.1053/jpnu.2002.127573
131. Sourdif J. Predictors of nurses’ intent to stay at work in a university health center. Nurs Health Sci. 2004;6(1):59–68. https://doi.org/10.1111/j.1442-2018.2003.00174.x
132. Lynn MR, Redman RW. Faces of the nursing shortage: influences on staff nurses’ intentions to leave their positions or nursing. J Nurs Adm. 2005;35(5):264–270. https://doi.org/10.1097/00005110-200505000-00010
133. Park HH, Park KS, Yom YH, Kim KH. [Impact of clinical nurses’ power and empowerment on job satisfaction and organizational commitment]. Taehan Kanho Hakhoe Chi. 2006;36(2):244–254. Korean. https://doi.org/10.4040/jkan.2006.36.2.244
134. Han SS, Moon SJ, Yun EK. Empowerment, job satisfaction, and organizational commitment: comparison of permanent and temporary nurses in Korea. Appl Nurs Res. 2009;22(4):e15–20. https://doi.org/10.1016/j.apnr.2009.06.004
135. Kim EK, Hwang JI. Characteristics associated with intent to stay among Quality Improvement nurses. Int Nurs Rev. 2011;58(1):89–95. https://doi.org/10.1111/j.1466-7657.2010.00841.x
136. Pinho P, Albuquerque C. Influência do empenhamento organizacional e profissional dos enfermeiros nas estratégias de resoluçāo dos conflitos [Influence of organizational commitment and professional nurses in conflict resolution strategies]. Servir. 2013;58(1–2):103–116. Portuguese.
137. Zhao X, Sun T, Cao Q, Li C, Duan X, Fan L, Liu Y. The impact of quality of work life on job embeddedness and affective commitment and their co-effect on turnover intention of nurses. J Clin Nurs. 2013;22(5- 6):780–788. https://doi.org/10.1111/j.1365-2702.2012.04198.x
138. Choi HG, Ahn SH. [Influence of Nurse Managers’ Authentic Leadership on Nurses’ Organizational Commitment and Job Satisfaction: Focused on the Mediating Effects of Empowerment]. J Korean Acad Nurs. 2016;46(1):100–108. Korean. https://doi.org/10.4040/jkan.2016.46.1.100
139. Negussie N, Berehe C. Factors affecting performance of public hospital nurses in Addis Ababa region, Ethiopia. J Egypt Public Health Assoc. 2016;91(1):26–30. https://doi.org/10.1097/01.EPX.0000480931.63648.9b
140. Gupta V, Agarwal UA, Khatri N. The relationships between perceived organizational support, affective commitment, psychological contract breach, organizational citizenship behaviour and work engagement. J Adv Nurs. 2016;72(11):2806–2817. https://doi.org/10.1111/jan.13043
141. Perreira T, Berta W, Ginsburg L, Barnsley J, Herbert M. Insights into nurses’ work: Exploring relationships among work attitudes and work-related behaviors. Health Care Manage Rev. 2018;43(4):315–327. https://doi.org/10.1097/HMR.0000000000000151
142. Huyghebaert T, Gillet N, Audusseau O, Fouquereau E. Perceived career opportunities, commitment to the supervisor, social isolation: Their effects on nurses’ well-being and turnover. J Nurs Manag. 2019;27(1):207–214. https://doi.org/10.1111/jonm.12666
143. Al-Ahmadi H. Factors affecting performance of hospital nurses in Riyadh Region, Saudi Arabia. Int J Health Care Qual Assur. 2009;22(1):40–54. https://doi.org/10.1108/09526860910927943
144. Han SS, Sohn IS, Kim NE. [New nurse turnover intention and influencing factors]. J Korean Acad Nurs. 2009;39(6):878–887. Korean. https://doi.org/10.4040/jkan.2009.39.6.878
145. Vagharseyyedin SA. An integrative review of literature on determinants of nurses’ organizational commitment. Iran J Nurs Midwifery Res. 2016;21(2):107–117. https://doi.org/10.4103/1735-9066.178224
146. McGillis Hall L, Lalonde M, Dales L, Peterson J, Cripps L. Strategies for retaining midcareer nurses. J Nurs Adm. 2011;41(12):531–537. https://doi.org/10.1097/NNA.0b013e3182378d6c
147. Sjöberg A, Sverke M. The interactive effect of job involvement and organizational commitment on job turnover revisited: a note on the mediating role of turnover intention. Scand J Psychol. 2000;41(3):247–252. https://doi.org/10.1111/1467-9450.00194
148. Mrayyan MT. Hospital organizational climates and nurses’ intent to stay: differences between units and wards. Contemp Nurse. 2008;27(2):223–236. https://doi.org/10.5555/conu.2008.27.2.223
149. Liou SR. Nurses’ intention to leave: critically analyse the theory of reasoned action and organizational commitment model. J Nurs Manag. 2009;17(1):92–99. https://doi.org/10.1111/j.1365-2834.2008.00873.x
150. Chen SY, Wu WC, Chang CS, Lin CT, Kung JY, Weng HC, Lin YT, Lee SI. Organizational justice, trust, and identification and their effects on organizational commitment in hospital nursing staff. BMC Health Serv Res. 2015;15:363. https://doi.org/10.1186/s12913-015-1016-8
151. Sveinsdóttir H, Ragnarsdóttir ED, Blöndal K. Praise matters: the influence of nurse unit managers’ praise on nurses’ practice, work environment and job satisfaction: a questionnaire study. J Adv Nurs. 2016;72(3):558–568. https://doi.org/10.1111/jan.12849
152. Rodwell J, Ellershaw J. Fulfill Promises and Avoid Breaches to Retain Satisfied, Committed Nurses. J Nurs Scholarsh. 2016;48(4):406–413. https://doi.org/10.1111/jnu.12215
153. Attree M. Patients’ and relatives’ experiences and perspectives of ‘Good’ and ‘Not so Good’ quality care. J Adv Nurs. 2001;33(4):456–466. https://doi.org/10.1046/j.1365-2648.2001.01689.x
154. Endo E, Miyahara T, Suzuki S, Ohmasa T. Partnering of researcher and practicing nurses for transformative nursing. Nurs Sci Q. 2005;18(2):138–145. https://doi.org/10.1177/0894318405274825
155. Cooper E. Creating a culture of professional development: a milestone pathway tool for registered nurses. J Contin Educ Nurs. 2009;40(11):501–508. https://doi.org/10.3928/00220124-20091023-07
156. Guerrero S, Chênevert D, Kilroy S. New Graduate Nurses’ Professional Commitment: Antecedents and Outcomes. J Nurs Scholarsh. 2017;49(5):572–579. https://doi.org/10.1111/jnu.12323
157. De Gieter S, Hofmans J, Pepermans R. Revisiting the impact of job satisfaction and organizational commitment on nurse turnover intention: an individual differences analysis. Int J Nurs Stud. 2011;48(12):1562–1569. https://doi.org/10.1016/j.ijnurstu.2011.06.007
158. Cleary M, Horsfall J. Integrity and mental health nursing: factors to consider. Issues Ment Health Nurs. 2013;34(9):673–677. https://doi.org/10.3109/01612840.2013.794179
159. Huynh T, Alderson M, Thompson M. Emotional labour underlying caring: an evolutionary concept analysis. J Adv Nurs. 2008;64(2):195–208. https://doi.org/10.1111/j.1365-2648.2008.04780.x
160. Tummers LG, Den Dulk L. The effects of work alienation on organisational commitment, work effort and work-to-family enrichment. J Nurs Manag. 2013;21(6):850–859. https://doi.org/10.1111/jonm.12159
161. Pendry PS. Moral distress: recognizing it to retain nurses. Nurs Econ. 2007;25(4):217–221.
162. Yildirim A, Yildirim D. Mobbing in the workplace by peers and managers: mobbing experienced by nurses working in healthcare facilities in Turkey and its effect on nurses. J Clin Nurs. 2007;16(8):1444–1453. https://doi.org/10.1111/j.1365-2702.2006.01814.x
163. Yildirim D. Bullying among nurses and its effects. Int Nurs Rev. 2009;56(4):504–511. https://doi.org/10.1111/j.1466-7657.2009.00745.x
164. Olender-Russo L. Creating a culture of regard: an antidote for workplace bullying. Creat Nurs. 2009;15(2):75–81. https://doi.org/10.1891/1078-4535.15.2.75
165. Schalk R. The influence of organizational commitment and health on sickness absenteeism: a longitudinal study. J Nurs Manag. 2011;19(5):596–600. https://doi.org/10.1111/j.1365-2834.2010.01170.x
166. Greenglass ER, Burke RJ. Hospital restructuring and burnout. J Health Hum Serv Adm. 2002;25(1):89–114.
167. Judkins SK, Ingram M. Decreasing stress among nurse managers: a long-term solution. J Contin Educ Nurs. 2002;33(6):259–264. https://doi.org/10.3928/0022-0124-20021101-06
168. Malagon-Aguilera MC, Suñer-Soler R, Bonmatí-Tomas A, Bosch-Farré C, Gelabert-Vilella S, Juvinyà-Canal D. Relationship between sense of coherence, health and work engagement among nurses. J Nurs Manag. 2019;27(8):1620–1630. https://doi.org/10.1111/jonm.12848
169. McGilton KS, McGillis Hall L, Boscart V, Brown M. Effects of director of care support on job stress and job satisfaction among long-term care nurse supervisors. Nurs Leadersh (Tor Ont). 2007;20(3):52–66. https://doi.org/10.12927/cjnl.2007.19288
170. Ho WH, Chang CS, Shih YL, Liang RD. Effects of job rotation and role stress among nurses on job satisfaction and organizational commitment. BMC Health Serv Res. 2009;9:8. https://doi.org/10.1186/1472-6963-9-8
171. Chen SY, Wu WC, Chang CS, Lin CT. Job rotation and internal marketing for increased job satisfaction and organisational commitment in hospital nursing staff. J Nurs Manag. 2015 Apr;23(3):297–306. https://doi.org/10.1111/jonm.12126. Epub 2013 Aug 26
172. Allen DE, de Nesnera A, Souther JW. Executive-level reviews of seclusion and restraint promote interdisciplinary collaboration and innovation. J Am Psychiatr Nurses Assoc. 2009 Aug;15(4):260–264. https://doi.org/10.1177/1078390309342749. PMID: 21665812
173. McAllister M, Stockhausen L. Using action research within a school of nursing: exposing tensions in ideologies. Aust J Adv Nurs. 2001;18(4):15–22.
174. Merkeley Keith K, Fraser Askin D. Effective collaboration: the key to better healthcare. Nurs Leadersh (Tor Ont). 2008;21(2):51–61. https://doi.org/10.12927/cjnl.2008.19875
175. Grube JA, Piliavin JA, Turner JW. The courage of one’s conviction: when do nurse practitioners report unsafe practices? Health Commun. 2010;25(2):155–164. https://doi.org/10.1080/10410230903544944
176. Altuntas S, Baykal U. Relationship between nurses’ organizational trust levels and their organizational citizenship behaviors. J Nurs Scholarsh. 2010;42(2):186–194. https://doi.org/10.1111/j.1547-5069.2010.01347.x
177. English B, Chalon C. Strengthening affective organizational commitment: the influence of fairness perceptions of management practices and underlying employee cynicism. Health Care Manag (Frederick). 2011;30(1):29–35. https://doi.org/10.1097/HCM.0b013e3182078ae2
178. Mark G, Smith AP. Occupational stress, job characteristics, coping, and the mental health of nurses. Br J Health Psychol. 2012;17(3):505–521. https://doi.org/10.1111/j.2044-8287.2011.02051.x
179. Schadenhofer P, Kundi M, Abrahamian H, Blasche G, Stummer H, Kautzky-Willer A. Job-related meaningfulness moderates the association between over-commitment and emotional exhaustion in nurses. J Nurs Manag. 2018;26(7):820–832. https://doi.org/10.1111/jonm.12602
180. Estes BC. Abusive supervision and nursing performance. Nurs Forum. 2013;48(1):3–16. https://doi.org/10.1111/nuf.12004
181. Cogin JA, Ng JL, Lee I. Controlling healthcare professionals: how human resource management influences job attitudes and operational efficiency. Hum Resour Health. 2016;14(1):55. https://doi.org/10.1186/s12960-016-0149-0
182. Bastos MA. O processo de socialização dos enfermeiros em um centro de tratamento intensivo [The process of socialization of nurses at an intensive care center]. Rev Esc Enferm USP. 2001;35(3):291–299. Portuguese. https://doi.org/10.1590/s0080-62342001000300014
183. Rapps J, Riegel B, Glaser D. Testing a predictive model of what makes a critical thinker. West J Nurs Res. 2001;23(6):610–626. https://doi.org/10.1177/01939450122045410
184. Robinson-Walker C. The role of coaching in creating cultures of engagement. Semin Nurse Manag. 2002;10(3):150–156.
185. Lu H, While AE, Barriball KL. A model of job satisfaction of nurses: a reflection of nurses’ working lives in Mainland China. J Adv Nurs. 2007;58(5):468–479. https://doi.org/10.1111/j.1365-2648.2007.04233.x
186. Liou SR, Cheng CY. Building organizational commitment of Asian nurses in the United States. J Nurs Adm. 2008;38(1):8–10. https://doi.org/10.1097/01.NNA.0000295633.80345.74
187. Good L. Addressing hospital nurses’ fear of abandonment in a bioterrorism emergency. AAOHN J. 2007;55(12):493–498; quiz 499–500. https://doi.org/10.1177/216507990705501203
188. Liou SR, Tsai HM, Cheng CY. Measuring Asian nurses’ organizational commitment: a critical analysis of the psychometric properties of two organizational commitment instruments. Nurs Forum. 2013 AprJun;48(2):142–153. https://doi.org/10.1111/nuf.12013
189. Lu KY, Pan SM, Lee LL, Shia LY, Chang YY. The influence of professional commitment on turnover intention. Kaohsiung J Med Sci. 2001;17(7):364–371.
190. Shih FJ, Liao YC, Chan SM, Duh BR, Gau ML. The impact of the 9-21 earthquake experiences of Taiwanese nurses as rescuers. Soc Sci Med. 2002;55(4):659–672. https://doi.org/10.1016/s0277-9536(01)00194-0
191. Park WY, Yoon SH. [The mediating role of organizational citizenship behavior between organizational justice and organizational effectiveness in nursing organizations]. J Korean Acad Nurs. 2009 Apr;39(2):229–236. Korean. https://doi.org/10.4040/jkan.2009.39.2.229
192. Cheah WL, Giloi N, Chang CT, Lim JF. The Perception, Level of Safety Satisfaction and Safety Feedback on Occupational Safety and Health Management among Hospital Staff Nurses in Sabah State Health Department. Malays J Med Sci. 2012;19(3):57–63.
193. Memarian R, Ahmadi F, Vaismoradi M. The leadership concept in Iranian nursing. Int Nurs Rev. 2008;55(1):48–54. https://doi.org/10.1111/j.1466-7657.2007.00587.x
194. Ravari A, Bazargan-Hejazi S, Ebadi A, Mirzaei T, Oshvandi K. Work values and job satisfaction: a qualitative study of Iranian nurses. Nurs Ethics. 2013;20(4):448–458. https://doi.org/10.1177/0969733012458606
195. Nasrabadi AN, Forooshani ZS, Rafiee F. Altruism the Essense of the Iranian Nurses’ Job Satisfaction: A Qualitative Study. Glob J Health Sci. 2016;8(8):50269. https://doi.org/10.5539/gjhs.v8n8p13
196. Trevizan MA, Mendes IA, Hayashida M, de Godoy S, Nogueira MS. La búsqueda del compromiso actitudinal: tendencia de la conducta ética del enfermero gerente [The search for attitudinal commitment: tendency in the manager nurse’s ethical behavior]. Rev Esc Enferm USP. 2009;43(3):721–725. Portuguese. https://doi.org/10.1590/s0080-62342009000300031
197. Pesut B, Fowler M, Reimer-Kirkham S, Taylor EJ, Sawatzky R. Particularizing spirituality in points of tension: enriching the discourse. Nurs Inq. 2009;16(4):337–346. https://doi.org/10.1111/j.1440-1800.2009.00462.x
198. Kagan I, Itzhaki M, Melnikov S. Patriotism, organizational commitment and nurses’ intention to report for work in emergencies. Int Nurs Rev. 2017;64(4):468–475. https://doi.org/10.1111/inr.12395
199. Antia BE, Bertin FD. Multilingualism and healthcare in Nigeria: a management perspective. Commun Med. 2004;1(2):107–117. https://doi.org/10.1515/come.2004.1.2.107
200. Timmermans K. Developing countries and trade in health services: which way is forward? Int J Health Serv. 2004;34(3):453–466. https://doi.org/10.2190/323D-0VJ3-XC58-VXHU
201. London L, Baldwin-Ragaven L. Human rights and health: challenges for training nurses in South Africa. Curationis. 2008;31(1):5–18. https://doi.org/10.4102/curationis.v31i1.898
202. Anyangwe SC, Mtonga C. Inequities in the global health workforce: the greatest impediment to health in sub-Saharan Africa. Int J Environ Res Public Health. 2007;4(2):93–100. https://doi.org/10.3390/ijerph2007040002
203. Adzei FA, Atinga RA. Motivation and retention of health workers in Ghana’s district hospitals: addressing the critical issues. J Health Organ Manag. 2012;26(4-5):467–485. https://doi.org/10.1108/14777261211251535
204. Kasper J, Bajunirwe F. Brain drain in sub-Saharan Africa: contributing factors, potential remedies and the role of academic medical centres. Arch Dis Child. 2012;97(11):973–979. https://doi.org/10.1136/archdischild-2012-301900
205. Rodríguez-Madrid MN, Pastor-Moreno G, Albert-Lopez E, PastorValero M. “You knew you had to be there, it had to be done”: Experiences of health professionals who faced the COVID-19 pandemic in one public hospital in Spain. Front Public Health. 2023;11:1089565. https://doi.org/10.3389/fpubh.2023.1089565
206. Langster HJ, Cutrer S. A Scoping Review of the Impact of Downsizing on Survivors. J Nurs Adm. 2021;51(6):329–333. https://doi.org/10.1097/NNA.0000000000001022
207. Soto-Rubio A, Giménez-Espert MDC, Prado-Gascó V. Effect of Emotional Intelligence and Psychosocial Risks on Burnout, Job Satisfaction, and Nurses’ Health during the COVID-19 Pandemic. Int J Environ Res Public Health. 2020;17(21):7998. https://doi.org/10.3390/ijerph17217998
208. Gander P, O’Keeffe K, Santos-Fernandez E, Huntington A, Walker L, Willis J. Development and evaluation of a matrix for assessing fatigue-related risk, derived from a national survey of nurses’ work patterns. Int J Nurs Stud. 2020;112:103573. https://doi.org/10.1016/j.ijnurstu.2020.103573
209. Jun J, Ojemeni MM, Kalamani R, Tong J, Crecelius ML. Relationship between nurse burnout, patient and organizational outcomes: Systematic review. Int J Nurs Stud. 2021;119:103933. https://doi.org/10.1016/j.ijnurstu.2021.103933
210. Atalla ADG, El-Ashry AM, Mohamed SMS. The influence of job enrichment on job embeddedness and sick presenteeism among nurses. Int Nurs Rev. 2025;72(2):e13043. https://doi.org/10.1111/inr.13043
211. Rodríguez-Fernández M, Herrera J, de Las Heras-Rosas C. Model of Organizational Commitment Applied to Health Management Systems. Int J Environ Res Public Health. 2021;18(9):4496. https://doi.org/10.3390/ijerph18094496
212. Renkema M, de Leede J, Van Zyl LE. High-involvement HRM and innovative behaviour: The mediating roles of nursing staff’s autonomy and affective commitment. J Nurs Manag. 2021;29(8):2499–2514. https://doi.org/10.1111/jonm.13390
213. Gong Z, Van Swol LM, Wang X. Study on the Relationship between Nurses’ Mentoring Relationship and Organizational Commitment. Int J Environ Res Public Health. 2022;19(20):13362. https://doi.org/10.3390/ijerph192013362
214. McCamey D. Making space and taking space: Promoting inclusion and belonging, a crucial imperative for nurse practitioner organizations. J Am Assoc Nurse Pract. 2023;35(9):531–533. https://doi.org/10.1097/JXX.0000000000000938
215. Gibson I, Kerins C, Foley L, Hynes L, Byrne M, Murphy AW, Reardon CM, McEvoy JW, Meade O. Factors influencing implementation of digital cardiac rehabilitation: A qualitative analysis of health workers perspectives. HRB Open Res. 2024;7:50. https://doi.org/10.12688/hrbopenres.13929.1
216. Sommer D, Wilhelm S, Wahl F. Nurses’ Workplace Perceptions in Southern Germany-Job Satisfaction and Self-Intended Retention towards Nursing. Healthcare (Basel). 2024;12(2):172. https://doi.org/10.3390/healthcare12020172
217. Adam D, Berschick J, Schiele JK, Bogdanski M, Schröter M, Steinmetz M, Koch AK, Sehouli J, Reschke S, Stritter W, Kessler CS, Seifert G. Interventions to reduce stress and prevent burnout in healthcare professionals supported by digital applications: a scoping review. Front Public Health. 2023;11:1231266. https://doi.org/10.3389/fpubh.2023.1231266
218. Mather CA, Cummings EA, Gale F. Advancing mobile learning in Australian healthcare environments: nursing profession organisation perspectives and leadership challenges. BMC Nurs. 2018;17:44. https://doi.org/10.1186/s12912-018-0313-z
219. Watson AL. Ethical considerations for artificial intelligence use in nursing informatics. Nurs Ethics. 2024;31(6):1031–1040. https://doi.org/10.1177/09697330241230515
220. Jeon HG, Jang KS, Kim EA. [The Influence of Diversity Management of Nursing Organization on Organizational Commitment: Double Mediating Effect of Diversity Sensitivity Orientation and Positive Nursing Organizational Culture]. J Korean Acad Nurs. 2024;54(3):403–417. Korean. https://doi.org/10.4040/jkan.23120
221. Morrison V, Hauch RR, Perez E, Bates M, Sepe P, Dans M. Diversity, Equity, and Inclusion in Nursing: The Pathway to Excellence Framework Alignment. Nurs Adm Q. 2021;45(4):311–323. https://doi.org/10.1097/NAQ.0000000000000494
222. Logroño KJ, Al-Lenjawi BA, Singh K, Alomari A. Assessment of nurse’s perceived just culture: a cross-sectional study. BMC Nurs. 2023;22(1):348. https://doi.org/10.1186/s12912-023-01478-4
223. Ito A, Sasaki M, Yonekura Y, Ogata Y. Impact of organizational justice and manager’s mental health on staff nurses’ affective commitment: A multilevel analysis of the work environment of hospital nurses in Japan-Part II (WENS-J-II). Int J Nurs Stud Adv. 2023;5:100137. https://doi.org/10.1016/j.ijnsa.2023.100137
224. Buss J, Arnold D. Communicative action, a path through the dissonance between nursing and corporate healthcare values. Nurs Inq. 2023;30(4):e12581. https://doi.org/10.1111/nin.12581
225. Lee AG, Carter KD. Managing the new mandate in resident education: a blueprint for translating a national mandate into local compliance. Ophthalmology. 2004;111(10):1807–1812. https://doi.org/10.1016/j.ophtha.2004.04.021
226. Choi SO. [The development of an organizational socialization process model for new nurses using a system dynamics approach]. Taehan Kanho Hakhoe Chi. 2005;35(2):323–335. Korean. https://doi.org/10.4040/jkan.2005.35.2.323
227. Callaghan L. The use of collaboration in personal outcomes. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2006;19(4-5):384–399. https://doi.org/10.1108/09526860610680030
228. Hsu MY, Kernohan G. Dimensions of hospital nurses’ quality of working life. J Adv Nurs. 2006;54(1):120–131. https://doi.org/10.1111/j.1365-2648.2006.03788.x
229. Schrems BM. Mind the gaps in ethical regulations of nursing research. Nurs Ethics. 2013;20(3):336–347. https://doi.org/10.1177/0969733012462051
230. Hofmeyer A, Marck PB. Building social capital in healthcare organizations: thinking ecologically for safer care. Nurs Outlook. 2008;56(4):145–151.e2. https://doi.org/10.1016/j.outlook.2008.01.001
Об авторах
К. В. КузьминРоссия
Кузьмин Константин Викторовичg/10.1016/s1060-135x(97 — кандидат исторических наук, доцент; руководитель Координационного научно-методического центра по социальной работе в системе здравоохранения Свердловской области
ул. Репина, д. 2а, г. Екатеринбург, 620014
Л. Е. Петрова
Россия
Петрова Лариса Евгеньевна — кандидат социологических наук, доцент, профессор кафедры социокультурного развития территории
ул. Культуры, д. 3, г. Екатеринбург, 620012
В. С. Харченко
Россия
Харченко Вера Сергеевна — кандидат социологических наук, зав. кафедрой медиакоммуникаций
ул. Мира, д. 19, г. Екатеринбург, 620062
Рецензия
Для цитирования:
Кузьмин К.В., Петрова Л.Е., Харченко В.С. Организационная приверженность среднего медицинского персонала: определение понятия и специфика измерений (обзор зарубежных публикаций). Кубанский научный медицинский вестник. 2025;32(5):96-120. https://doi.org/10.25207/1608-6228-2025-32-5-96-120
For citation:
Kuzmin K.V., Petrova L.E., Kharchenko V.S. Organizational commitment of nursing staff: Definition of the concept and specifics of measurement (review of foreign publications). Kuban Scientific Medical Bulletin. 2025;32(5):96-120. (In Russ.) https://doi.org/10.25207/1608-6228-2025-32-5-96-120








































