Scroll to:
Efficacy Evaluation of Combination Therapy in Patients with Generalized Periodontitis According to the Index Estimation of Periodontal Status: Experimental Randomized Single-Arm Study
https://doi.org/10.25207/1608-6228-2023-30-4-18-27
Abstract
Background. Treatment and prevention of inflammatory periodontal diseases represent a serious general medical and social problem, which remains relevant due to the significant prevalence of periodontitis among the population, as well as the associated loss of teeth and the negative impact of periodontal foci of infection on the body as a whole. Chronic generalized periodontitis is difficult to treat: it is only possible to achieve periods of remission. Therefore, it is of great theoretical and practical importance to develop further ways to improve methods for treating inflammatory-dystrophic damage of periodontal tissues in chronic generalized periodontitis.
Objective. To perform an index estimation of treatment efficacy in patients with moderately severe chronic generalized periodontitis.
Methods. An experimental randomized single-arm study was conducted examining 204 patients diagnosed with moderately severe chronic generalized periodontitis. Patient examination and data analysis were carried out at the Dentistry Department of the Stavropol State Medical University and the Department for General Practice Dentistry of the Kuban State Medical University in 2021–2022. The study included patients aged 35 to 65 years diagnosed with moderately severe chronic generalized periodontitis. Patients with somatic diseases in the decompensation stage were not eligible for the study. The patients were randomly divided into three groups (closed-envelope method). Group 1 was treated using conventional methods. As well as conventional therapy, Group 2 was prescribed vitamin D (Aquadetrim® at a dose of 5000 IU once per day while monitoring vitamin D blood level). The third group of patients was prescribed conventional therapy along with the developed pharmacotherapy, which included vitamin D (Aquadetrim® at a dose of 5000 IU once per day), vitamin A (3.44% oil solution of retinol acetate at a dose of 50 000 IU, 15 min after a morning meal), and 2-ethyl-6-methyl-3-hydroxypyridine (Mexidol® at a dose of 125 mg twice a day). In each patient, the treatment efficacy was analyzed in adjacent oral cavity segments (split-mouth design) according to clinical pocket depth, attachment loss, and bleeding on probing. Also, the authors used the X-ray index to assess the condition of osseous structures and the simplified oral hygiene index. The specified indices were estimated prior to treatment and at one and 12 months following treatment. The statistical analysis of study results was performed using Excel Microsoft Office 2016 (Microsoft, USA).
Results. The obtained data indicate that the immediate clinical outcomes (after one month) of combination therapy in patients from all three groups were approximately the same. However, the efficacy of treatment measures in the long-term period (12 months) was different, as evidenced by the dynamics of index values. Only in Group 3 patients, the full implementation of pharmacotherapeutic measures as part of the combination therapy of periodontitis ensured a stable therapeutic effect throughout the entire period of observation.
Conclusion. The data obtained 12 months following treatment indicate that the additional prescription of the developed pharmacotherapy contributed to prompt inflammation relief in periodontal tissues, providing a stable treatment outcome and long-term remission.
Keywords
For citations:
Romanenko A.R., Sirak S.V., Shamanova Z.K., Verevkina Yu.V., Bykova N.I., Lenev V.N., Arutyunov A.V. Efficacy Evaluation of Combination Therapy in Patients with Generalized Periodontitis According to the Index Estimation of Periodontal Status: Experimental Randomized Single-Arm Study. Kuban Scientific Medical Bulletin. 2023;30(4):18-27. https://doi.org/10.25207/1608-6228-2023-30-4-18-27
INTRODUCTION
The combination therapy of chronic periodontitis patients includes non-surgical and surgical methods [1][2][3]; however, regardless of the chosen strategy, the main focus should be on eliminating the main etiological factor—bacterial biofilm [4][5][6]. The conventional therapy of chronic generalized periodontitis (CGP) includes removal of supra- and subgingival dental calculus; closed (at a depth of less than 5 mm) and open (at a depth of over 5 mm) curettage of pathological pockets with the removal of granulation tissues; cleaning of pockets with antiseptic solutions; antimicrobial and anti-inflammatory therapy, both local (films, gels, and therapeutic dressings) and systemic [6][7][8]. Orthopedic measures are most often aimed at achieving balanced articulation, functional selective grinding, dental splinting, and the restoration of masticatory efficiency; however, the outcome of treatment largely depends on therapeutic interventions [8][9][10]. The therapeutic pharmacotherapy of periodontitis is based on using antiseptics in the form of oral baths, applications, and irrigation, as well as anti-inflammatory and antimicrobial drugs [8][9][10]. Under the conditions of chronic sensitization in the presence of a focus of microbial infection in the periodontium, the role of the organism’s immune defense cannot be underestimated, which requires additional measures to enhance immunity, including medication [14][15]. In recent years, data have been obtained on the high efficacy of photodynamic therapy [16][17], ozone [18], and pharmacotherapy using trace elements, vitamins, and antioxidants [19][20]. Despite the variety of treatment methods and the wide range of pharmacotherapeutic measures, there are not enough indications to choose one or another type.
The study aims to perform an index estimation of treatment efficacy in patients with moderately severe CGP.
METHODS Study design
The present study followed the design of a clinical experimental randomized single-arm study. The study included 204 patients diagnosed with moderately severe CGP who were randomly divided into three groups.
Eligibility criteria
Inclusion criteria
Age from 35 to 65 years, moderately severe CGP, and voluntary informed consent.
Exclusion criteria
Ages of under 35 and over 65, presence of oncological diseases, diseases in the decompensation stage, neurological and psychiatric diseases, and allergic history.
Removal criteria
Refusal to continue the participation in the study; refusal to comply with the doctor’s recommendations.
Study conditions
The patients were observed at the Dentistry Department of the Stavropol State Medical University and at the Department for General Practice Dentistry of the Kuban State Medical University.
Study duration
The study was conducted between September 2021 to September 2022.
Medical interventions
Participant selection involved an oral examination by a dentist to assess the periodontal status of the patient. History taking was performed to exclude general health contraindications. All patients were advised to undertake a complete blood count and a blood test to determine vitamin D levels. In addition, an X-ray examination was conducted, i.e., plain radiography.
The first group of patients was treated using only conventional methods: professional oral hygiene with removal of all supra- and subgingival dental calculus; curettage; cleaning of periodontal pockets with antiseptic solutions (0.05% Miramistin solution); application of therapeutic periodontal dressings with metronidazole (Periodontal Pack, Soe Pack, Voco Pack, and Septo Pack) and Diplen-denta films; antimicrobial and anti-inflammatory therapy (macrolides in combination with antiprotozoal drugs) received until the symptoms of inflammation disappear.
In addition to the conventional treatment methods specified above, the second group of patients was prescribed vitamin D (Aquadetrim® at a dose of 5000 IU once per day while monitoring vitamin D blood level for a month).
As well as the conventional therapy (identical to that received by groups 1 and 2), the third group of patients was prescribed the developed pharmacotherapy, which included vitamin D (Aquadetrim® at a dose of 5000 IU once per day for one month), vitamin A (3.44% oil solution of retinol acetate at a dose of 50000 IU, 15 min after a morning meal for one month), and 2-ethyl-6-methyl-3-hydroxypyridine (Mexidol® at a dose of 125 mg twice per day for one month).
Study outcomes
Main study outcome
Efficacy analysis of combination periodontal therapy relying on the index estimation of pathological changes in periodontal tissues using the periodontal and gingival indexes, as well as the X-ray index to assess the osseous structure condition, in the long-term (12 months).
Additional study outcomes
No additional outcomes are intended.
Methods for recording outcomes
When estimating the periodontal index (PI, A. Russel, 1956), the periodontal status of each tooth was assessed. Here, the degree of inflammation, tooth mobility, and the periodontal pocket depth were taken into account. Then, the mean index for all teeth (points) was calculated. When determining the gingival index (GI, H. Loe and J. Silness, 1967), the gingiva surrounding the following teeth was examined: 16, 12, 24, 44, 32, and 36. The condition of gingiva surrounding each tooth was assessed in four areas: distal surface, mesial surface, center of the vestibular surface, and center of the lingual surface. The examination was performed visually and using a periodontal bulbous probe. The mean score was determined for each tooth; then the values for all teeth were summed and divided by the number of examined teeth.
In order to determine the oral hygiene index (OHI-S, J.C. Green, J.R. Vermillion, 1964), the buccal surfaces of 16 and 26, the labial surfaces of 11 and 31, as well as the lingual surfaces of 36 and 46, were examined by moving the tip of the probe from the incisal edge toward the gingiva. The presence of plaque (staining of the specified surfaces with Lugol’s iodine) and calculus was assessed in each tooth (in points).
In order to determine the X-ray index, a plain radiograph was taken; then, the degree of osseous tissue damage in the area of each tooth was assessed (in points) by placing a graduated grid (reference) on the radiograph.
Confounding factors that can affect the therapy efficacy and the estimated indices include the specifics of outpatient reception (i.e., the physician cannot control antibacterial medication compliance), the recommended pharmacotherapy, as well as the use of local antiseptics and the quality of individual oral hygiene following professional oral hygiene and curettage.
Randomization
Patients were sampled via the sequential method. Upon inclusion in the study, each patient was assigned a group number according to the order in which they sought medical care. After assigning 65 patients to Groups 1, 2, and 3 each, the remaining patients were placed in Group 3. Thus, all patients were divided into three groups: Group 1 (n = 65, aged 39 to 65 years, 29 males, 36 females); Group 2 (n = 65, aged 35 to
62 years, 32 males, 33 females); Group 3 (n = 74, aged 36 to 65 years, 39 females, 35 males).
Data anonymity assurance
Upon receipt and further processing of patient source data, we anonymized and delocalized them, if necessary. For studies, a new key code was introduced for patient parameters, without disclosing the connection between the code and personal data.
Statistical procedures
Principles behind sample size determination
The sample size was not determined in advance.
Statistical methods
The statistical analysis of study results was performed using Excel Microsoft Office 2016 (Microsoft, USA); the normality of the distribution was checked using the Kolmogorov–Smirnov test; Fisher’s analysis of variance was performed; when comparing mean values, Student’s t-test and Newman-Keuls test were used for independent measurements and paired measurements, respectively. The dynamics of examined indices in the context of treatment were evaluated both in absolute units (points) in the form of the mean value and its error (M±m) and in percentage with respect to the baseline. The proportions were compared using the Chi-squared test for a four-way or an arbitrary-sized table. Differences were considered statistically significant at an error level of p < 0.05.
RESULTS
Sampling
The sampling was conducted according to the inclusion and exclusion criteria. In order to conduct this study, three groups were formed. Group 1 included 65 patients; Group 2 comprised 65 patients; Group 3 consisted of 74 patients. All patients were observed for the entire duration of the study (Fig. 1).
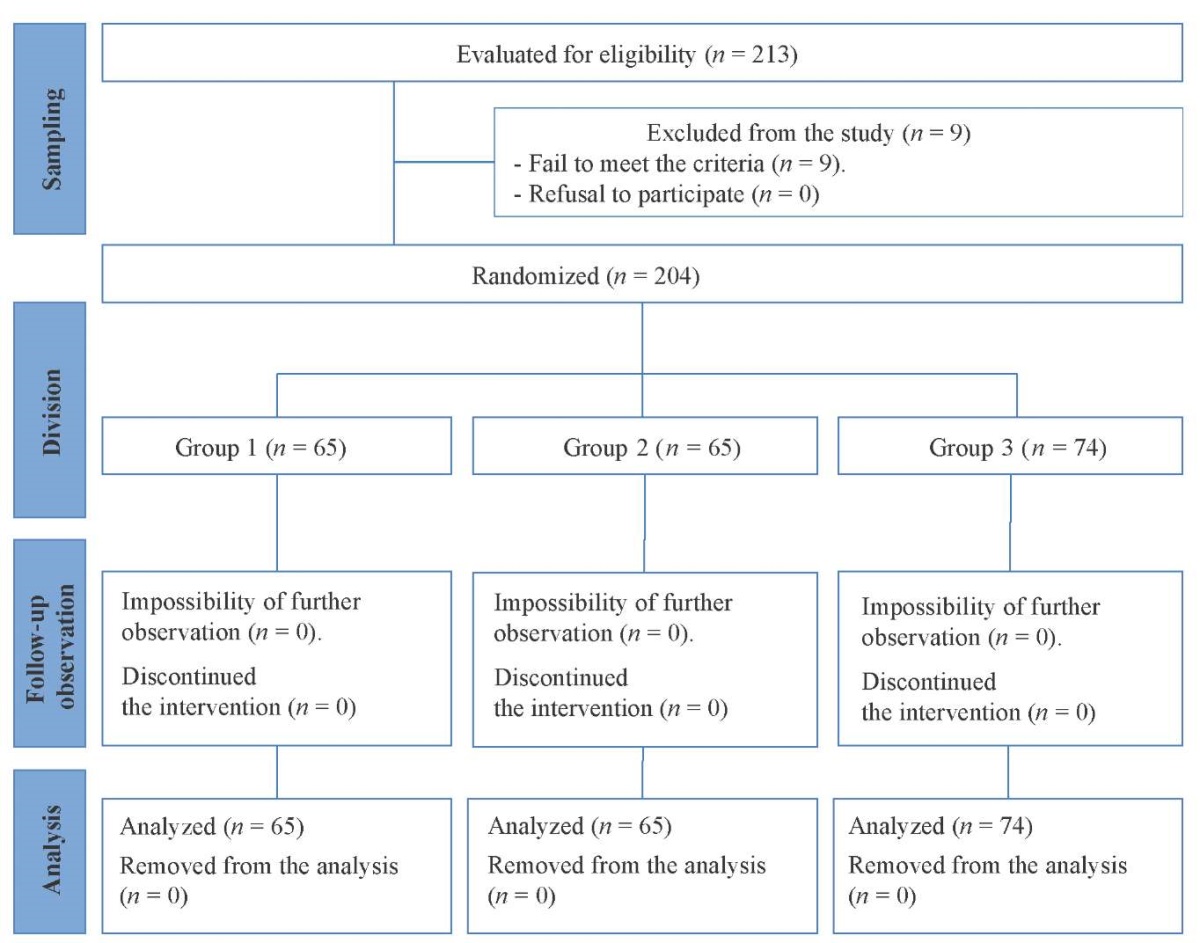
Fig. 1. Block diagram of the study design
Note: The block diagram was created by the authors
(as per CONSORT recommendations).
Рисунок 1. Блок-схема дизайна исследования
Примечание: блок-схема выполнена авторами
(согласно рекомендациям CONSORT).
Characteristics of the study sample (groups)
All patients were divided into three groups: 1) Group 1 (n = 65; aged 39 to 65 years; 29 males and 36 females); mean age of (51.20±1.04) years; the hypothesis of normality is not rejected (p = 0.134); 2) Group 2 (n = 65; aged 35 to 62 years; 32 males and 33 females); mean age of (49.80±2.30) years; the normality hypothesis is not rejected (p = 0.551); 3) Group 3 (n = 74; aged 36 to 65 years; 39 females and 35 males); mean age of (54.40±1.02) years; the normality hypothesis is not rejected (p = 0.227). The conducted analysis of variance revealed no statistically significant difference in mean age between the three groups (p = 0.148 according to F-test). Pairwise age comparison between groups (for Groups 1 and 2, p = 0.518; for Groups 1 and 3, p = 0.112; for Groups 2 and 3, p = 0.093) also showed the statistical insignificance of differences in mean values. Age-wise, the groups were comparable.
The proportions of males and females in the groups were compared. An analysis of contingency tables according to the Chi-squared test revealed no statistically significant difference between the proportions of males and females in the groups (p = 0.870). Pairwise sex comparison between the groups (for Groups 1 and 2, p = 0.599; for Groups 1 and 3, p = 0.752; for Groups 2 and 3, p = 0.820) also showed the statistical insignificance of differences in the proportions. In terms of sex, the groups were comparable.
Main study result
The initial periodontal status in patients from the compared groups exhibited virtually no differences. As a result of using various combination therapy regimens, the clinical condition of the periodontium improved in all groups. However, the treatment efficacy proved to be different, as evidenced by the index score dynamics.
Prior to treatment, no statistically significant difference was found for the PI of patients in the compared groups (analysis of variance and pairwise comparison yielded values of p > 0.05). After initiation of CGP therapy, certain differences were revealed in the examined groups: the greatest PI decrease corresponding to low inflammation intensity was observed in Group 3 patients, i.e., (3.14 ± 0.62) points, which was statistically significantly lower than the score of (5.48 ± 0.56) points of Group 1 patients (p = 0.025) and the score of Group 2 amounting to (5.24 ± 0.58) points (p = 0.018), as well as lower than the score of Group 3 prior to treatment estimated at (5.56 ± 0.57) points (p = 0.020). The PI comparison between Group 1 (control) and Group 2 patients showed no statistically significant difference (p = 0.435). This indicates a substantial reduction in the inflammatory process in periodontal tissues after initiation of therapy in Group 3 patients (Fig. 2).
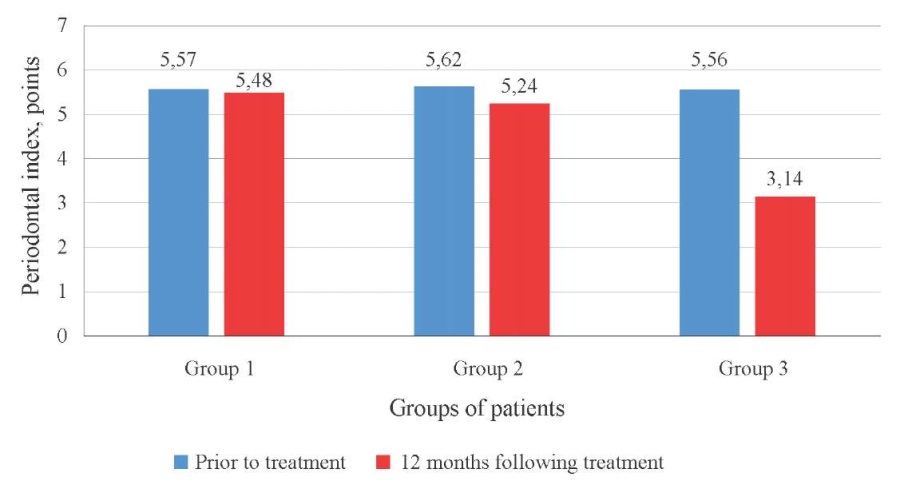
Fig. 2. Periodontal index (PI) in chronic periodontitis patients prior to treatment
and 12 months following treatment in different groups
Note: The figure was created by the authors.
Рис. 2. Значения пародонтального индекса (PI)
у больных хроническим пародонтитом до лечения
и через 12 месяцев после лечения в различных группах
Примечание: рисунок выполнен авторами.
No significant differences in X-ray index level were found between Groups 1 and 2 neither prior to nor following treatment (p > 0.05). However, Group 3 patients exhibited a significant increase in this index from (0.499 ± 0.055) points to (0.618 ± 0.085) points or a 23.8% increase (p < 0.05) following treatment, which was not observed in the other groups (p > 0.05). This indicates a faster normalization of the periodontal osseous tissue condition in Group 3 patients (Fig. 3).
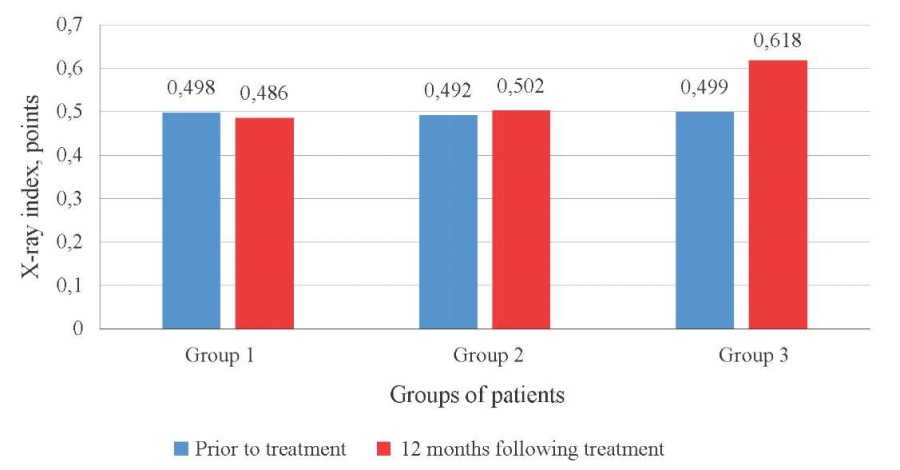
Fig. 3. X-ray index in chronic periodontitis patients prior to treatment
and 12 months following treatment in different groups
Note: The figure was created by the authors.
Рис. 3. Значения рентгенологического индекса (X-ray index)
у больных хроническим пародонтитом до лечения
и через 12 месяцев после лечения в различных группах
Примечание: рисунок выполнен авторами.
The comparative study of GI dynamics in patients with moderately severe periodontitis confirmed that in the context of ongoing treatment, this inflammatory index decreases significantly in all examined groups at one month (for all groups, p < 0.05). In Group 1, the index decreased from (1.98 ± 0.02) to (1.14 ± 0.02); in Group 2, the index decreased from (2.09 ± 0.03) to (1.25 ± 0.02); in Group 3, the index decreased from (2.05 ± 0.03) to (1.22 ± 0.02). In analyzing GI one month after initiation of therapy, it was found to have decreased by about the same amount (about 40%) in patients from all three groups.
и через 12 месяцев после лечения в различных группах Примечание: рисунок выполнен авторами.
A high GI sensitivity was noted to changes in the inflammation intensity in the periodontium, which manifested itself in the differences in the index values at one month and 12 months after initiation of therapy. In the control Group 1, the GI score increased from (1.14 ± 0.02) to (1.55 ± 0.03) points (p < 0.05) over a period of time ranging from one month to 12 months after initiation of treatment, indicating recurrence of the inflammatory process. In Group 2 patients, no statistically significant changes were found (p > 0.05), while in Group 3 patients, the GI score indicated a significant inflammation reduction from (1.22 ± 0.02) to (0.72 ± 0.01) points (p < 0.01).
Twelve months after initiation of treatment, a significant difference in the mean GI score was observed in all groups (p < 0.05) as compared to its pre-treatment level (Fig. 4).
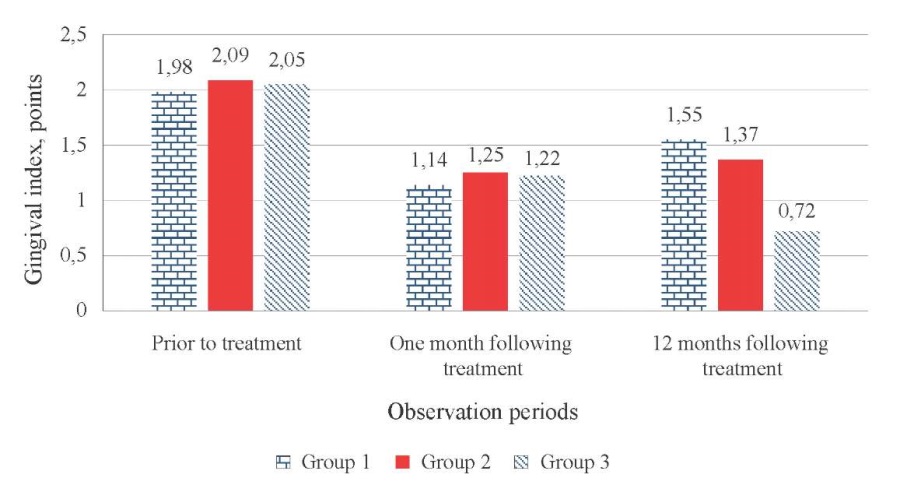
Fig. 4. Gingival index (GI) in chronic periodontitis patients
from the compared groups at different observation periods
Note: The figure was created by the authors.
Рис. 4. Значения гингивального индекса GI
у больных хроническим пародонтитом
в сравниваемых группах в различные сроки наблюдения
Примечание: рисунок выполнен авторами.
Thus, at 12 months after initiatio n of treatment, GI remained statistically significantly reduced as compared to the baseline value in patients from all three groups. The obtained data revealed a GI reduction of only 21.7% in the control group, 34.4% in Group 2, and 64.9% in Group 3.
Such dynamics of the GI indicate that the greatest efficacy was achieved in Group 3 using pharmacotherapy, along with a lasting therapeutic effect, although prior to the initiation of treatment, the GI score in patients of this group was high.
Twelve months after initiation of therapy, the OHI-S score exhibited dynamics (index decrease) similar to that of the GI, which is an important indication of the relationship between oral hygiene and the inflammatory process in the periodontium (Fig. 5).
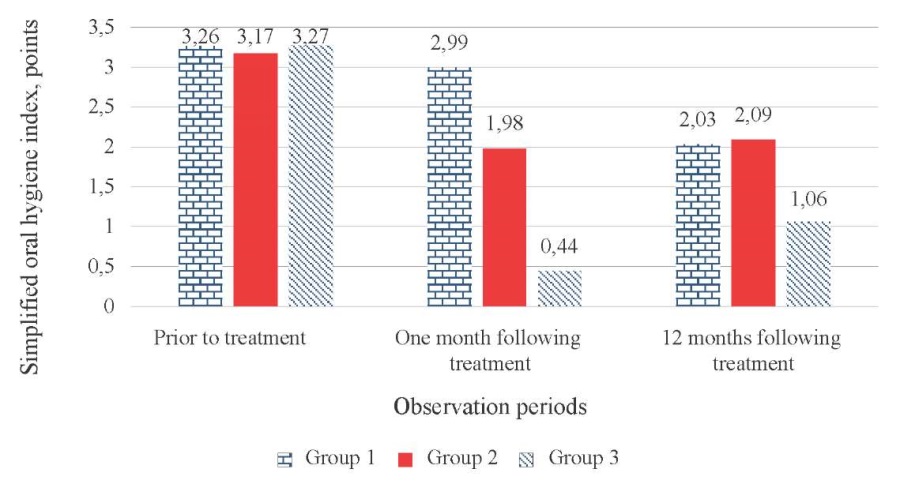
Fig. 5. Simplified oral hygiene index (OHI-S) score
in chronic periodontitis patients from the compared groups
at different observation periods
Note: The figure was created by the authors.
Рис. 5. Значения упрощенного индекса гигиены полости рта (OHI-S)
у больных хроническим пародонтитом в сравниваемых группах
в различные сроки наблюдения
Примечание: рисунок выполнен авторами.
At one month after initiation of therapy, the OHI-S score decreased by 86.5% in Group 3 patients as compared to its initial level, i.e., from (3.27 ± 0.04) to (0.44 ± 0.02) points (p < 0.001); in Group 1 and Group 2 patients, the decrease in this index was more moderate, amounting to 8.3% for Group 1 and 37.5% for Group 2 (p < 0.05).
As indicated by the estimation of the simplified oral hygiene index (OHI-S) 12 months after initiation of therapy, Group 3 was characterized by the lowest OHI-S level as compared to other groups, i.e., (1.06 ± 0.07) points, which was statistically significantly lower than those of Groups 1 and 2 — (2.03 ± 0.09) points (p < 0.01) and (2.09 ± 0.09) points (p < 0.01), respectively.
Thus, the comparative analysis of the considered indices in CGP patients treated according to different regimens showed the advantage of using the developed pharmacotherapy as part of the treatment regimen for chronic periodontitis.
Only Group 3 showed an improvement in the condition of periodontal osseous tissue (23.8% increase in the X-ray index as compared to the baseline, p < 0.05), whereas the application of conventional therapy methods in the control group or additional prescription of vitamin D in Group 2 patients resulted in the maintenance of the low baseline level of the X-ray index.
Only Group 3 patients showed a pronounced (nearly 1.77 times) PI decrease as compared to the baseline.
A significant improvement in GI and OHI-S scores was observed in patients from all groups (p < 0.05). However, after one to 12 months following treatment, GI and OHI-S scores tend to increase in the control group and Group 2 patients, which shows that the treatment methods used in these groups as less effective. Only in Group 3 patients, the full implementation of pharmacotherapeutic measures as part of complex periodontitis therapy ensured a stable therapeutic effect throughout the entire period of observation.
Additional study results
No additional results were obtained during the study.
Adverse events
No adverse events were observed during the study.
DISCUSSION
Research limitations
Not identified.
Extrapolation
The obtained study results can be used in practical dentistry when carrying out combination therapy for patients with periodontal diseases. In addition, the study showed that the proposed pharmacological measures produce a stable therapeutic effect, leading to long-term remission, which can improve the patient’s quality of life.
Summary of the main study result
The estimation of periodontal and X-ray indices can be used in conducting the studies as a way to objectively assess the state of periodontal tissues. The additional prescription of the developed pharmacotherapy including vitamin D (Aquadetrim® at a dose of 5000 IU one time per day), vitamin A (3.44% oil solution of retinol acetate at a dose of 50000 ME 15 min after a morning meal), and 2-ethyl-6-methyl-3-hydroxypyridine (Mexidol® at a dose of 125 mg two times per day) was found to produce a stable therapeutic effect, leading to longterm remission.
Discussion of the main study result
Periodontal diseases currently represent one of the common and complex pathologies in modern dentistry. A review of scientific works revealed that one of the leading factors in CGP development consists in the presence of pathogenic periodontal microflora that contributes to the occurrence of inflammatory processes in periodontal tissues [21][22]. The severity of inflammation and conducted therapy outcomes can be used to objectively estimate the commonly known indices used in this study [23][24]. Among the numerous treatment methods, the leading method in the combination CGP therapy is the therapeutic treatment with the use of various drugs, whose selection should be based on the degree and form of pathology, as well as the severity of CGP [25][26], which is consistent with the treatment outcome.
Summarizing the obtained data on index estimation, it can be noted that, irrespective of the prescribed regimen, the inflammation relief was observed in all three groups at one month after initiation of therapy. However, in the long-term follow-up period (12 months), the obtained therapeutic effect was not maintained in Groups 1 and 2. The study results indicate that the developed pharmacotherapy used together with conventional therapy in patients with moderately severe CGP contributes to inflammation relief and prolonged remission period. Provided that patients with relieved periodontal inflammation followed the recommended oral hygiene regimen, it was possible to normalize the main clinical scores of the periodontal status.
CONCLUSION
The study results revealed that conventional methods for the therapy of moderately severe chronic periodontitis reduce periodontal inflammation in the short term (one month); however, the obtained therapeutic effect cannot be maintained in the long-term follow-up period (12 months). The application of the developed pharmacotherapeutic measures as part of combination therapy contributes to a long-term remission of the disease in the context of complete cessation of attachment loss and condition improvement of periodontal osseous tissue.
The obtained data indicate that it is best to use the developed pharmacotherapeutic measures in the combination therapy of moderately severe generalized periodontitis, suggesting that this method should be more widely implemented in clinical practice.
References
1. Sanz-Martín I, Cha JK, Yoon SW, Sanz-Sánchez I, Jung UW. Longterm assessment of periodontal disease progression after surgical or non-surgical treatment: a systematic review. J Periodontal Implant Sci. 2019;49(2):60–75. https://doi.org/10.5051/jpis.2019.49.2.60
2. Herrera D, Retamal-Valdes B, Alonso B, Feres M. Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo-periodontal lesions. J Clin Periodontol. 2018;45 Suppl 20:S78– S94. https://doi.org/10.1111/jcpe.12941
3. Jepsen S, Caton JG, Albandar JM, Bissada NF, Bouchard P, Cortellini P, Demirel K, de Sanctis M, Ercoli C, Fan J, Geurs NC, Hughes FJ, Jin L, Kantarci A, Lalla E, Madianos PN, Matthews D, McGuire MK, Mills MP, Preshaw PM, Reynolds MA, Sculean A, Susin C, West NX, Yamazaki K. Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol. 2018;45 Suppl 20:S219–S229. https://doi.org/10.1111/jcpe.12951
4. Loos BG, Van Dyke TE. The role of inflammation and genetics in periodontal disease. Periodontol 2000. 2020;83(1):26–39. https://doi.org/10.1111/prd.12297
5. Cecoro G, Annunziata M, Iuorio MT, Nastri L, Guida L. Periodontitis, LowGrade Inflammation and Systemic Health: A Scoping Review. Medicina (Kaunas). 2020;56(6):272. https://doi.org/10.3390/medicina56060272
6. Van der Weijden GAF, Dekkers GJ, Slot DE. Success of non-surgical periodontal therapy in adult periodontitis patients: A retrospective analysis. Int J Dent Hyg. 2019;17(4):309–317. https://doi.org/10.1111/idh.12399
7. Hu X, Huang YY, Wang Y, Wang X, Hamblin MR. Antimicrobial Photodynamic Therapy to Control Clinically Relevant Biofilm Infections. Front Microbiol. 2018;9:1299. https://doi.org/10.3389/fmicb.2018.01299
8. Amos-Tautua BM, Songca SP, Oluwafemi OS. Application of Porphyrins in Antibacterial Photodynamic Therapy. Molecules. 2019;24(13):2456. https://doi.org/10.3390/molecules24132456
9. Di Stasio D, Romano A, Russo D, Fiori F, Laino L, Caponio VCA, Troiano G, Muzio LL, Serpico R, Lucchese A. Photodynamic therapy using topical toluidine blue for the treatment of oral leukoplakia: A prospective case series. Photodiagnosis Photodyn Ther. 2020;31:101888. https://doi.org/10.1016/j.pdpdt.2020.101888
10. Caccianiga G, Rey G, Baldoni M, Caccianiga P, Baldoni A, Ceraulo S. Periodontal Decontamination Induced by Light and Not by Heat: Comparison between Oxygen High Level Laser Therapy (OHLLT) and LANAP. Applied Sciences. 2021;11(10):4629. https://doi.org/10.3390/app11104629
11. Afrasiabi S, Partoazar A, Chiniforush N, Goudarzi R. The Potential Application of Natural Photosensitizers Used in Antimicrobial Photodynamic Therapy against Oral Infections. Pharmaceuticals (Basel). 2022;15(6):767. https://doi.org/10.3390/ph15060767
12. Romano A, Di Stasio D, Gentile E, Petruzzi M, Serpico R, Lucchese A. The potential role of Photodynamic therapy in oral premalignant and malignant lesions: A systematic review. J Oral Pathol Med. 2021;50(4):333–344. https://doi.org/10.1111/jop.13139
13. Petrini M, Spoto G, Scarano A, D’Arcangelo C, Tripodi D, Di Fermo P, D’Ercole S. Near-infrared LEDS provide persistent and increasing protection against E. faecalis. J Photochem Photobiol B. 2019;197:111527. https://doi.org/10.1016/j.jphotobiol.2019.111527
14. Butera A, Gallo S, Maiorani C, Molino D, Chiesa A, Preda C, Esposito F, Scribante A. Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters. Microorganisms. 2020;9(1):69. https://doi.org/10.3390/microorganisms9010069
15. Butera A, Gallo S, Pascadopoli M, Taccardi D, Scribante A. Home Oral Care of Periodontal Patients Using Antimicrobial Gel with Postbiotics, Lactoferrin, and Aloe Barbadensis Leaf Juice Powder vs. Conventional Chlorhexidine Gel: A Split-Mouth Randomized Clinical Trial. Antibiotics (Basel). 2022;11(1):118. https://doi.org/10.3390/antibiotics11010118
16. Stájer A, Kajári S, Gajdács M, Musah-Eroje A, Baráth Z. Utility of Photodynamic Therapy in Dentistry: Current Concepts. Dent J (Basel). 2020 May 7;8(2):43. https://doi.org/10.3390/dj8020043
17. Plotino G, Grande NM, Mercade M. Photodynamic therapy in endodontics. Int Endod J. 2019;52(6):760–774. https://doi.org/10.1111/iej.13057
18. Scribante A, Gallo S, Pascadopoli M, Soleo R, Di Fonso F, Politi L, Venugopal A, Marya A, Butera A. Management of Periodontal Disease with Adjunctive Therapy with Ozone and Photobiomodulation (PBM): A Randomized Clinical Trial. Photonics. 2022;9(3):138. https://doi.org/10.3390/photonics9030138
19. Lauritano D, Moreo G, Palmieri A, Vella FD, Petruzzi M, Botticelli D, Carinci F. Photodynamic Therapy Using 5-Aminolevulinic Acid (Ala) for the Treatment of Chronic Periodontitis: A Prospective Case Series. Applied Sciences. 2022:18;12(6):3102. http://dx.doi.org/10.3390/app12063102
20. Toczewska J, Konopka T. Activity of enzymatic antioxidants in periodontitis: A systematic overview of the literature. Dent Med Probl. 2019;56(4):419–426. https://doi.org/10.17219/dmp/112151
21. Dzampaeva ZV. Etiology And pathogenesis features of inflammatory periodontal diseases (Review). Kuban Scientific Medical Bulletin. 2017;5:103–110 (In Russ.). https://doi.org/10.25207/1608-6228-2017-24-5-103-110
22. Sabirova A, Akramov I, Ramazanova Z, Sergeeva V, Ibisheva L. Modern aspects of epidemiological issues of periodontal tissue diseases. The Scientific Heritage. 2021;73-2(73):31–38 (In Russ.). https://doi.org/10.24412/9215-0365-2021-73-2-31-38
23. Mikhailova IG, Moskovskiy AV, Karpunina AV, Urukov YuN, Moskovskaya OI, Shuvalova NV. Evaluation of index values in patients with mild or moderate chronic periodontitis. Pediatric dentistry and dental prophylaxis. 2020;20(4):310–315 (In Russ.). https://doi.org/10.33925/1683-30312020-20-4-310-315
24. Farkhshatova RR, Usmanova IN, Gerasimova LP. Clinical and x-ray features of periodontic tissues in patients with gingival recession. Actual problems in dentistry. 2020;16(1):81–86 (In Russ.). https://doi.org/10.18481/2077-7566-20-16-1-81-86
25. Sablina S, Elovicova T, Griroriev S, Khromtsova O, Zakroeva A, Yepishova A, Karaseva V, Mirsaev T, Dorokhina K. The role of vitamin D in maintaining oral health. Literature review. Actual problems in dentistry. 2020;16(4)25–34 (In Russ.). https://doi.org/10.18481/20777566-20-16-4-25-34
26. Losev FF, Krechina EK, Ivanova EV, Kuksa EYu, Guseva IE. The use of photodynamic therapy in the complex treatment of chronic generalized moderate periodontitis. Stomatologiya. 2023;102(2):11–15 (In Russ.). https://doi.org/10.17116/stomat202310202111
About the Authors
A. R. RomanenkoRussian Federation
Alina R. Romanenko — Teaching Assistant, Dentistry Department
Mira str., 310, Stavropol, 355017
S. V. Sirak
Russian Federation
Sergei V. Sirak — Dr. Sci. (Med.), Prof., Head of the Dentistry Department
Mira str., 310, Stavropol, 355017
Z. K. Shamanova
Russian Federation
Zuhra K. Shamanova — postgraduate student, Department for General Practice Dentistry
Mitrofana Sedina str., 4, Krasnodar, 350063
Yu. V. Verevkina
Yuliya V. Verevkina — postgraduate student, Department for General Practice Dentistry
Mitrofana Sedina str., 4, Krasnodar, 350063
N. I. Bykova
Russian Federation
Natal’ya I. Bykova — Cand. Sci. (Med.), Assoc. Prof., Department for Pediatric Dentistry, Orthodontics, and Oral and Maxillofacial Surgery
Mitrofana Sedina str., 4, Krasnodar, 350063
V. N. Lenev
Russian Federation
Vadim N. Lenev — Cand. Sci. (Med.), Assoc. Prof., Dentistry Department
Mira str., 310, Stavropol, 355017
A. V. Arutyunov
Russian Federation
Armenak V. Arutyunov — Dr. Sci. (Med.), Assoc. Prof., Head of the Department for General Practice Dentistry
Mitrofana Sedina str., 4, Krasnodar, 350063
Review
For citations:
Romanenko A.R., Sirak S.V., Shamanova Z.K., Verevkina Yu.V., Bykova N.I., Lenev V.N., Arutyunov A.V. Efficacy Evaluation of Combination Therapy in Patients with Generalized Periodontitis According to the Index Estimation of Periodontal Status: Experimental Randomized Single-Arm Study. Kuban Scientific Medical Bulletin. 2023;30(4):18-27. https://doi.org/10.25207/1608-6228-2023-30-4-18-27








































