Scroll to:
Gottron’s Carcinoid Papillomatosis: Case Report
https://doi.org/10.25207/1608-6228-2023-30-6-81-88
Abstract
Introduction. Gottron’s papillomatosis is a rare benign type of dermatosis with pseudoepitheliomatous hyperplasia of the epidermis, first described as an independent disease by the German dermatologist H.A. Gottron. Invasive epidermal growth and hyperkeratosis reveal no signs of malignancy. Chronic venous insufficiency and lymphedema can be associated with various secondary skin lesions: the formation of ulcers, hyperkeratosis and skin papillomatosis, as well as infectious complications. Skin papillomatosis may be a manifestation of paraneoplastic syndrome, which requires a careful differential diagnosis. Timely treatment of complications in a patient with concomitant somatic pathology performed by a multidisciplinary team of specialists is necessary to improve the prognosis. Considering the relative rarity of Gottron’s papillomatosis and the lack of awareness among practicing physicians regarding the differential diagnosis of this disease, we present this clinical analysis.
Description of a clinical case. Patient L., 42 years old (body mass index — 76.5 kg/m2) with chronic lymphovenous insufficiency, lymphedema, erysipelas of the right lower limb associated with unspecified skin papillomatosis, was urgently hospitalized in a health care institution “City Clinical Hospital No. 3” of Grodno (Republic of Belarus), consulted by a multidisciplinary team of clinicians including a therapist, a cardiologist, a dermatologist, an endocrinologist, an infectious disease specialist, and a surgeon. Taking into account the clinical status of the patient and the retrospective analysis of archival records of previous examinations performed on the patient in the health care institution “Grodno University Clinic”, the type of dermatosis was determined as Gottron’s papillomatosis of both lower extremities. In terms of the clinical diagnosis of the patient, complex therapy was initiated in a hospital setting, which was then continued at the outpatient stage.
Conclusion. Adequate long-term treatment of morbid obesity and chronic lymphovenous insufficiency is necessary to prevent serious complications. According to the academic literature, timely diagnosis of such a rare dermatosis as Gottron’s papillomatosis, as well as the prescription of adequate therapy determine the possibility of regression in the early stages of the disease.
Keywords
For citations:
Balabanovich T.I., Surmach K.M., Dziamidzik S.N., Budrevich V.V., Warnakulasuriya Fernando R.S. Gottron’s Carcinoid Papillomatosis: Case Report. Kuban Scientific Medical Bulletin. 2023;30(6):81-88. https://doi.org/10.25207/1608-6228-2023-30-6-81-88
INTRODUCTION
Gottron’s carcinoid papillomatosis of skin is a rare type of dermatosis, accounting for approximately 60 cases in the academic literature across the world [1][2].
There are no epidemiological data of Gottron’s carcinoid papillomatosis in Belarus, and, therefore, this fact does not allow behavior analysis the of the disease in our population. In our opinion, the incidence and prevalence of Gottron’s carcinoid papillomatosis in Belarus is poorly understood, probably because of the difficulty in accurately identifying and documenting such cases. According to some sources, Gottron’s carcinoid papillomatosis is precancerous condition that can transform to the squamous cell carcinoma. Dating back to 2010–2019, the Belorussian Cancer Registry reported a high increase in morbidity (46.7%) of skin cancer among Belarussian population1. Further research is required to fill existing gaps in understanding the epidemiology of Gottron’s carcinoid papillomatosis and tendencies in its incidence across Belarus.
According to modern concepts, Gottron’s carcinoid papillomatosis is considered as a benign type of dermatosis characterized by pseudoepitheliomatous hyperplasia of epidermis. This dermatosis is more common in men over 40 with various pathological conditions and predisposing factors associated with chronic inflammation, such as other persistent dermatosis types, chronic skin ulcers, primary or secondary lymphedema, impaired blood circulation and venous insufficiency, human papilloma viruses and so on. Some comorbid diseases such as diabetes mellitus, obesity, and psoriasis are associated with a host of disorders that can also affect symptoms, function, and prognosis of Gottron’s carcinoid papillomatosis [3][4]. The disease is characterized by the decades-long, slowly progressive course with no necrotic-ulcerative changes. The disease predominantly affects lower extremities. However, cases of the skin lesions on the upper extremities and chest have been described. The location of the lesions can be both symmetrical and asymmetrical. Patients commonly reveal a combination of lower extremity edemas due to lymphatic stasis and papillomatosis cutis. Papillomatosis cutis lymphostatica as well as Gottron’s carcinoid papillomatosis is a severe complication of chronic lymphedema and venous insufficiency characterized by hyperkeratotic and papillomatous changes as well as skin lesions [5]. Practitioners should have basic knowledge and skills to detect Gottron’s carcinoid papillomatosis in patients and use available diagnostic methods to determine the diagnosis.
CASE PRESENTATION
Patient information
The 42-year-old morbidly obese male was admitted to the intensive care unit of the Grodno Municipal Clinical Hospital No. 3 on February 4, 2023, with complaints of severe unrelenting pain in right lower limb, swelling of the entire right extremity and oozing of fluid from the right lower limb, inability to move independently, burning sensation and fullness in the legs, fatigue and weakness, shortness of breath, sweating, and daytime sleepiness.
Anamnesis morbi: The first signs of lipedema and varicose veins occurred 10 years earlier. Severe varicosities of the leg veins remained untreated for a long period and led to stasis dermatitis, lymphedema with multiple polypoid conglomerates on the skin of the lower extremities, secondary ulcerations, and so in 2022, the patient applied to the surgical department of the Health Care Institution “Grodno University Clinic”. This fact of the past case history was known only from the words of the patient (the patient had no hospital epicrisis) and, unfortunately, the patient was not able to give a clear view of his illness and prescribed medications. After that period, the patient did not have any medical consultation and was taking some drugs from time to time. The patient felt worse from the middle of January, 2023. The following complaints developed: pain in the right lower extremity, enlargement of the right leg, fever (temperature up to 39 °C). Domestically he used non-steroidal anti-inflammatory drugs for pain syndrome, but didn’t remember doses and names. The patient refused to cooperate with doctors and refused hospitalization as well as skin care procedures. On February 4, 2023, the patient was hospitalized by his wife calling the ambulance due to intensity of symptoms (severe weakness, febrile fever with chills, intensive pain (7 according to numeric rating scale).
Anamnesis vitae: The patient had a longstanding history of hypertension and obesity. His antihypertensive treatment consisted of bisoprolol for 10 mg/day, valsartan for 160 mg/day, atorvastatin for 20 mg/day, sodium levothyroxine for 75 mcg/day. No oral anticoagulants or antiplatelet drugs were administered. The patient was diagnosed with morbid obesity and autoimmune thyroiditis, subclinical hypothyroidism (no medical treatment received), and adenoma in the right adrenal gland. Diabetes mellitus type 2 was treated by oral administration of metformin for 1000 mg. Patient had hereditary history of arterial hypertension. No bad habits or allergies.
Clinical Findings
The patient was admitted in a severe state. He was in a forced (left lateral) position with body temperature 37,0 °C. Height — 198 cm, weight — 300 kg, body mass index (BMI) — 76,5 kg/m2. Waist circumference — 140 cm. According to the numeric rating scale for pain the patient selected score 7. The color of the face was pink, while his lips were slightly cyanotic. The respiratory rate was 20 breaths/min. Lungs auscultation revealed decreased vesicular breath sounds under the scapulars. Heart auscultation revealed diminished S1 on the apex, accentuated S2 on the aortic valve point, no heart murmurs. The pulse was arrhythmic, 86 beats per minute. The blood pressure was 140/90 mmHg.
The right lower leg was severely increased in size (hip circumference at the upper third was 165 cm, circumference of the middle third of the tibia was 87 cm), purple-cyanotic, edematous, painful with erythematous rash, widespread presence of trophic changes and papillomatosis, erosive defects up to 5 cm (Figure 1a-b).
A foul-smelling yellow-whitish secretion expressed from the lesions; the gray-yellow crusts were present in some areas. The Kaposi—Stemmer sign was positive. The capillary refill was less than two seconds. The left lower extremity was painless, but revealed edema and papillomatosis, too. Peripheral pulses were palpated bilaterally.
The primary diagnosis
Chronic venous insufficiency of both legs, C4, Ep, A p, d, Pr, 04.02.2023; LI. Chronic lymphedema, grade III. Papillomatosis cutis? Erysipelas in the right lower extremity? Ischemic heart disease: atherosclerotic cardiosclerosis. Persistent atrial fibrillation, normasystolic type, EHRA IIa. Atherosclerosis of aorta, coronary vessels. Heart failure: functional class III (NYHA), objective assessment C, Vasilenko-Strazhesko stage II-A. Arterial hypertension, grade ІІІ, risk 4. Obesity, grade III (BMI = 76,5 kg/m2). Obesity hypoventilation syndrome? Diabetes Mellitus type 2, compensation. Autoimmune thyroiditis. Adrenal adenoma (no hormonal activity).
Timeline
The chronology of disease in patient L. is depicted on the Figure 2.
Diagnostic Assessment
Laboratory investigations (conducted at the health care institution “City Clinical Hospital No. 3” in Grodno, on February 4, 2023; reference values are indicated in brackets)
Complete blood count: red blood cells (RBC) count 4.02×1012/L ((4.63–6.08)×1012/L); hemoglobin 115 g/L (135–175 g/L); mean corpuscular volume (MCV) 80.5 fl (79.0–92.2 fl); mean cell hemoglobin (MCH) 25.4 pg (25.6–32.2 pg); mean corpuscular hemoglobin concentration (MCHC) 31.6 g/dl (32.2–36.5 g/dl); white blood cells (WBC) count 12.6×109/L ((4.23–9.07)×109/L): neutrophils: band cells 6% (1–5%), segmented cells 78% (40–68%), lymphocytes 8.0% (21,8–53.1%), monocyte 3.0% (5.3–12.2%), eosinophils 5 (1–5%), platelets 434×109/L (150–450×109/L), erythrocyte sedimentation rate (ESR) 54 mm/h (1–15 mm/h).
Biochemical blood test: total protein 68 g/L (65–85 g/L), albumin 34 g/L (34–48 g/L), urea 4.8 mmol/L (1.7–8.3 mmol/L), creatinine 1.4 mg/dL (0.6–1.1 mg/dL), estimated glomerular filtration rate (eGFR) 64 ml/min/1.73 m2 (≥120 ml/min/1.73 m2), C-reactive protein (CRP) 46.2 mg/dL (0–6 mg/dL), alanine aminotransferase (ALT) 57 U/L (5–42 U/L), aspartate aminotransferase (AST) 41 U/L (5–37 U/L), glucose 6.5 mmol/L (3.5–6.2 mmol/L), total bilirubin 0.74 mg/dL (0.29–1.17 mg/dL), total cholesterol 6.0 mmol/L (3.1–5.2 mmol/L), high density lipoproteins (HDL) 0.8 mmol/l (1.03–1.55 mmol/l), low density lipoproteins (LDL) 2.15 mmol/l (2.6–4.1 mmol/l), triglycerides (Tg) 2.52 mmol/l (0.1–1.7 mmol/l), potassium 4.6 mmol/L (3.2–5.6 mmol/L), sodium 142 mmol/L (130–155 mmol/L), total calcium 2.2 mmol/L (2.0–2.6 mmol/L), chlorides 102 mmol/L (95–110 mmol/L), ferritin 405 mcg/L (20–250 mcg/L), serum ferrum 17.1 mcmol/L (11.6–31.3 mcmol/L).
Coagulation test: fibrinogen 7.2 g/L (2.0–4.0 g/L), D-dimer test 1158 ng/mL (500 ng/mL), activated partial thromboplastin time (APTT) 33.2 sec (28.0–40.0 sec), international normalised ratio (INR) 1.12 (0.90–1.30).
Arterial blood gas analysis: hypercapnic acidosis (PaСO2 of 56 mm Hg; pH = 7,31); SaO2 = 92,1% at room temperature.
Urine analysis: physical properties-color — yellow (straw yellow), transparence (transparent), acidic reaction (acidic), specific gravity — 1022 g/L (1012–1022 g/L); chemical properties — protein count 0,09 g/L (absent (up to 0,033 g/L); erythrocytes — 1–3 in sight (single in sight), leukocytes — 8 in sight (up to 3 single in sight), bacteria absent, mucus — absent (absent).
Other investigations
Glycated hemoglobin A1c: 6.40% (4.27–6.07%). Thyroid hormones: Free thyroxine (free Т4) = 12.4 ng/dL (0.7–1.8 ng/dL), antibodies to thyroid peroxidase > 525 mIU (0–34 mIU), thyroid stimulating hormone (TSH) = 5.0 mlU/L (0.3–3.0 mlU/L). Progesterone 3.3 ng/ml (0.2–1.4 ng/ml), cortisol (8 am) = 234.5 nmol/L (171–536 nmol/L), testosterone 3.3 nmol/L (10.4–41.6 nmol/L), prolactin 395.7 mU/ml (86.0–324.0 mU/ml), follicle stimulating hormone (FSH) = 8.3 mU/ml (1.0–11.0 mU/ml), luteinizing hormone (LH) = 7.5 mU/l (0.8–8.4 mU/ml).
Syphilis serology negative. Polymerase chain reaction identified no human papillomavirus. Specific laboratory investigation for streptococci — positive bacteriological skin culture: Streptococcus pyogenes (A). Negative syphilis and human immunodeficiency virus (HIV) screening tests.
Microscopic investigations: Microscopy for fungal infection of the scraping of the epidermis of the skin was performed twice (both negative).
Instrumental investigations (conducted at the health care institution “City Clinical Hospital No. 3” in Grodno)
Electrocardiogram (ECG) 04.02.2023: atrial fibrillation, normasystolic type. Heart rate = 86/min. Left axis deviation. Amplitude signs of LV hypertrophy. CHA2DS2-VASc scale = 4; HAS-BLED scale = 2.
Chest radiography (04.02.2023) revealed an enlarged heart shadow with pulmonary venous hypertension and slight signs of pulmonary congestion.
Bilateral venous duplex ultrasound (04.02.2023) showed negative results for deep vein thrombosis (DVT), and computed tomography (CT) angiogram revealed bilateral lower extremity superficial reflux with enlargement of bilateral greater saphenous veins and numerous superficial varicosities below the calf soft tissues along the greater saphenous vein courses bilaterally.
Bilateral arterial duplex ultrasound (04.02.2023) was without abnormalities.
Transthoracic echocardiography (07.02.2023): echo-signs of atherosclerosis of the aorta. Dilatation of both atria of the heart. Left ventricular (LV) myocardial hypertrophy. Left ventricular ejection fraction = 50%. Valvular regurgitation (mitral, tricuspid) 2 degree. Moderate pulmonary hypertension (44 mmHg).
Ultrasound of the abdomen (07.02.2023): enlargement of the liver (right lobe is 259 mm, left is 132 mm), v. portae 10 mm, spleen size is 158×54 mm. No pancreas visualization. Kidney: right — 138×69 mm, left — 136×66 mm, parenchyma thickness: 14–15 mm. Contour: uneven. Echostructure: heterogeneous. The projection of the right adrenal gland presents adenoma of 45×30 mm.
Ultrasound of the thyroid gland (05.02.23) revealed fibrous diffuse changes in visible areas, without clear data for nodular formations.
Sonographic assessment of the breast (05.02.23) showed a glandular-stromal complex with the presence of ducts is determined, with a total size of about 50×25 mm on the right, 38×30 mm on the left side. There are lymph nodes up to 20 mm on the right, up to 12 mm on the left side of the inguinal regions.
Histological investigation (conducted at the health care institution “Grodno University Clinic”, 03.06.2022)
Histopathological analysis from archives of the medical record of the patient at the “Grodno University Clinic”: a skin fragment with hyperkeratosis, papillomatosis, pronounced pseudoepitheliomatous epidermal hyperplasia, acanthosis, the formation of epithelial strands penetrating into the deep layers of the dermis with the presence in the dermis of a large number of vessels of small caliber and focal lymphoid infiltration. No atypical cells (Fig. 3).
The final clinical diagnosis
Chronic venous insufficiency of both legs, C4, Ep, Ap, d, Pr, 04.02.2023; LI. Chronic lymphedema, grade III. Gottron’s carcinoid papillomatosis. Erysipelas in the right lower extremity. Ischemic heart disease: atherosclerotic cardiosclerosis. Permanent atrial fibrillation, normasystolic type, EHRA IIa. Atherosclerosis of aorta, coronary vessels. Heart failure with preserved ejection fraction (50%): functional class III (NYHA), objective assessment C, Vasilenko—Strazhesko stage II-A. Moderate pulmonary hypertension (44 mmHg). Arterial hypertension grade ІІІ, risk 4. Obesity, grade III (BMI = 76.5 kg/m2). Obesity-hypoventilation syndrome. Diabetes mellitus type 2, compensation. Chronic tubulointerstitial nephritis. Chronic kidney disease c2 (eGFR by CKD-EPI on 04.02.23 = 64 ml/min/1.73 m2). Metabolic associated fatty liver disease. Autoimmune thyroiditis, subclinical hypothyroidism. Gynecomastia. Adrenal adenoma (no hormonal activity).
Differential Diagnosis
Squamous cell carcinoma, spinocellular epithelioma, warty tuberculosis, chronic vegetative pyoderma and chromomycosis are the most important diseases for differential diagnosis. Paraneoplastic cutaneous manifestations (cutaneous papillomatosis) recognition and identification can enable early diagnosis and treatment of associated neoplasms [6].
A significant risk factor of squamous cell cancer is old age, together with cumulative sun exposure, fair skin, prolonged immunosuppression and previous skin cancer diagnoses. Invasive carcinoma generally present as a persistent ulcer. Dermatoscopy and microscopy enhanced the diagnosis. The main histological features are parakeratosis, hyperkeratosis with an epidermis characterized by the presence of disordered maturation with atypical keratinocytes through all the epidermal layers, individual cell keratinization, pleomorphism of nuclei, atypical mitoses, and multinucleated tumor cells [7]. Spinocellular epithelioma is invasive malignant tumor with cytonuclear abnormalities [8].
Chronic ulcerative vegetative pyoderma has unique clinical and histological characteristics. These lesions begin as a single furunculoid purple abscess, nodule or plaque. They are most commonly present on the trunk. Pseudoepitheliomatous hyperplasia and diffuse neutrophilic infiltration with microabscess formation are present in dermis [9].
In atypical variants of cutaneous tuberculosis, one has to rely on investigations like histopathology, bacilli culture, or polymerase chain reaction for confirmatory diagnosis. Histopathological investigations show nodular or diffuse tuberculoid granulomatous inflammation involving the papillar and reticular dermis. The granuloma consists of lymphocytes, plasma cells, epithelioid cells; with or without Langhan’s or foreign body giant cells. The overlying epidermis shows moderate to severe hyperplasia (pseudoepitheliomatous hyperplasia) [10].
Chromoblastomycosis can be proved by direct microscopy (reveals muriform, sclerotic bodies). Occasional dematiaceous hyphae may be associated with the muriform bodies in the material. The specimens with the highest likelihood of a positive result are those from lesions with the so-called “black dots” that are visible on the lesion’s surface [11].
In case of Gottron’s papillomatosis, papillomatous warts are detected which protrude 1 cm above the skin level and they are covered with vegetation. The grooves between the expansions are filled with a yellowish-white sticky mass with an unpleasant smell, and in some areas the gray-yellow crusts. Biopsy with histological examination can prove diagnosis (acanthosis with enlarged epithelial growth, penetrating deep into the dermis, no atypical cells).
Medical interventions (Therapeutic intervention)
On the day of admission (04.02.2023) patient was prescribed empirically 2 g intravenous ceftriaxone once daily, rozuvastatin 20 mg/day orally, rivaroxaban 20 mg/day orally, lansoprazole 30 mg/day orally, levothyroxine natrium 75 mcg/day. The patient remained hemodynamically stable, and blood pressure and heart rate were controlled with bisoprolol 10 mg/day orally, valsartan 160 mg/day orally, torasemide 10 mg/day orally. It was made a decision to administer dapagliflozin 10 mg/day orally, additionally to metformin 1000 mg bid orally. The patient was given non-invasive ventilation (the O2 flow rate was 5 l/min). It was recommended bed rest with elevated position of the legs. Surgery was consulted thereafter, was adviced conservative treatment without surgical excision. The patient reported right lower extremity pain (according to numeric rating scale for pain the patient had 7), for which aceclofenac was administered. Initially, the detoxication therapy was started with 400,0 mg intravenous meglumine sodium succinate once daily. The patient’s immunodeficiency was corrected with 1 million units of interleukin-2 intravenous. Vitamin therapy was initiated with the complex of vitamins B1, B6, B12. Ultraviolet irradiation was used as a treatment method. The antibiotics were continued until the erythema and pain disappeared (course of 14 days). Erosion care treatment with chlorhexidine application was performed, along with complex application of “Betamethasonum+Gentamicinum+Clotrimazolum” ointment. Compression wraps were used to reduce swelling.
Follow-up and outcomes
The patient had a good response to antibacterial treatment: within 72 hours, there was no more fever, pain and skin signs were reduced. Such positive dynamics supported a diagnosis of erysipelas [12]. During the first 3 days after the admission, patients’ laboratory indicators of inflammation (CRP, WBC, procalcitonin) increased followed by a gradual decrement in follow-up days (table 1). On the 1s–8th days of the disease patient’s general condition was of moderate severity. The patient was evaluated by a dermatologist and a surgeon. The conservative therapy started consisting of antimicrobials, diuretics, and topical agents, to reduce edema and infection, recommendations for weight reduction and treatment of concomitant diseases, the use of compression bandaging, mechanical massage, exercise, and elevation, physiotherapy [5][13]. On the day 18th of the disease the general condition of the patient was satisfactory. The erosions on the intact areas healed. The patient was stable and afebrile.
The patient was discharged on the 18th day after admission and got instructions to follow up concerning his adequate long-term outpatient treatment and medical monitoring.
Treatment prospects
The prognosis is doubtful. Medical recommendations can help in reducing significant symptoms, but it is not a definitive cure and the majority of such patients typically reveal similar symptoms and ulcer manifestations again. The patient continues his out-patient treatment. The patient has not been readmitted in-patient to the point of writing the present paper.
Patient’s opinion
In the patient’s opinion, poorly managed dermatologic problems associated with cardio-vascular disorders and diabetes mellitus together with his uncooperation may lead to the delayed treatment effect and such complications as he had previously.
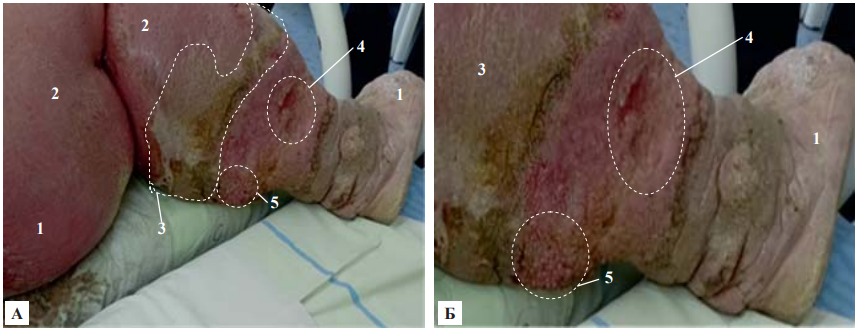
Figs. 1 А, Б. Patient L. Right lower leg. 1 — elephantism, 2 — erysipelas, 3 — lymphedema and lipodermatosclerosis, 4 — erosions, 5 — papillomatosis.
Note: photographs taken by the authors.
Рис. 1 А, Б. Пациент Л. Голень правой ноги. 1 — элефантизм, 2 — рожа, 3 — лимфедема и липодерматосклероз, 4 — эрозии, 5 — папилломатоз.
Примечание: фотографии выполнены авторами.
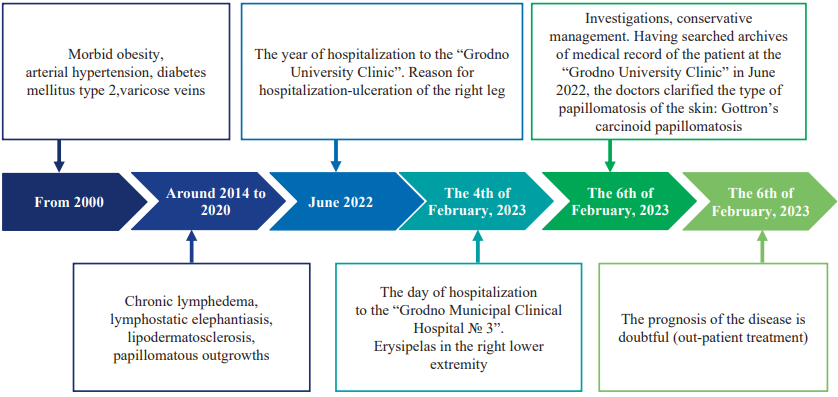
Fig. 2. Course of the disease in patient L.: key events and prognosis
Note: The timeline flowchart was created by the authors (in accordance with the CARE recommendations).
Рис. 2. Течение болезни у пациента Л.: ключевые события и прогноз
Примечание: блок-схема временной шкалы выполнена авторами (согласно рекомендациям CARE).
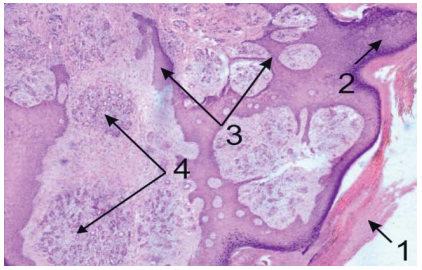
Fig. 3. Histology of a skin fragment of the right leg (hematoxylin-eosin; magnification ×50): 1 — hyperkeratosis, 2 — papillomatosis, 3 — severe pseudoepitheliomatous hyperplasia of the epidermis, the formation of epithelial strands penetrating the deep dermis layers, 4 — a large number of small caliber vessels and focal lymphoid infiltration
Note: photographs taken by the authors.
Рис. 3. Гистология фрагмента кожи правой ноги (гематоксилин-эозин; увеличение ×50): 1 — гиперкератоз, 2 — папилломатоз, 3 — выраженная псевдоэпителиоматозная гиперплазия эпидермиса, формирование эпителиальных тяжей, проникающих в глубокие слои дермы, 4 — большое количество сосудов мелкого калибра и очаговая лимфоидная инфильтрация
Примечание: фотографии выполнены авторами.
Table 1. Laboratory dynamics throughout the entire period of hospitalization
Таблица 1. Динамика лабораторных показателей на протяжении всего периода госпитализации
Laboratory parameters | Day of the disease | |||
04.02.2023 | 07.02.2023 | 14.02.2023 | 20.02.2023 | |
RBC, 1012/l | 4.2 | 4.8 | 5.2 | 4.6 |
Hemoglobin, g/l | 115 | 126 | 133 | 140 |
Platelets, 109/l | 434 | 406 | 328 | 395 |
WBC, 109/l | 12.6 | 11.5 | 6.9 | 6.4 |
ESR, mm/h | 54 | 51 | 37 | 22 |
Total protein, g/l | 68 | 60 | 62 | 66 |
Albumin, g/l | 34 | 33.8 | 36 | 41 |
Creatinine, mg/dl, | 1.4 | 1.58 | 1.33 | 1.24 |
CKD-EPI GFR, ml/min/1.73 m2 | 64 | 56 | 68 | 74 |
CRP, mg/dl | 46.2 | 43 | 34.5 | 20.2 |
ALT/AST, U/l | 57 / 41 | 60 / 49 | 53 /39 | 50/47 |
D-dimer, ng/ml | 1158 | 1010 | 897 | 780 |
Fibrinogen, g/l | 7.2 | 6.9 | 5.7 | 5.5 |
Procalcitonin, ng/ml | 0.90 | 0.50 | 0.09 | 0.06 |
Note: The table was compiled by the authors. Abbreviations: RBC — red blood cell count; WBC — white blood cell count; ESR — erythrocyte sedimentation rate; CKD-EPI GFR — CKD-EPI Equations for Glomerular Filtration Rate; ALT — alanine aminotransferase; AST — aspartate aminotransferase; CRP — C-reactive protein.
Примечание: таблица составлена авторами. Сокращения: RBC — количество эритроцитов; WBC — количество лейкоцитов; ESR — скорость оседания эритроцитов; CKD-EPI GFR — скорость клубочковой фильтрации (CKD–EPI калькулятор оценки); ALT — аланинаминотрансфераза; AST — аспартатаминотрансфераза; CRP — С-реактивный белок.
DISCUSSION
Gottron’s carcinoid papillomatosis is an extremely rare case [14][15]. It can be diagnosed based on its unique clinical picture and characteristic morphological changes. Nevertheless diagnostics errors are still common among practitioners due to rareness of this condition [1][4][15]. Lesions expressed as multiple papillomatosis and tumor like growths, oozing out of exudate between the foci, the presence of hyperkerotic and cortical layers on their surface. Dermatoscopy first used high technological method to diagnosis as well as pronounced pseudoepitheliomatous hyperplasia of the epidermis without the signs of atypia, papillomatosis, and acanthosis. By the opinions of most researchers’ priority is the prevention of previous dermatosis, including timely diagnostics and treatment of chronic skin diseases and other comorbid pathology [1][15].
CONCLUSION
Diagnosis and management of Gottron’s carcinoid papillomatosis developed in a comorbid patient with severe lymphovenous insufficiency complicated by erysipelas is a challenge for physicians. It may mimic other dermatologic conditions and thus requires a good level of diagnostic procedures based on the patient’s present and prior medical history. This situation requires clear decisions made by a multidisciplinary team of specialists.
1. Cancer in Belarus: numbers and facts. Analysis of data from the Belarusian cancer registry for 2010–2019. / A.E. Okeanov [et al.]; edited by O.G. Polyakova. Minsk: N.N. Alexandrova Republican Scientific and Practical Centre of OMR, 2020. P. 298.
Рак в Беларуси: цифры и факты. Анализ данных белорусского канцер-регистра за 2010–2019 гг. / А.Е. Океанов [и др.]; под ред. О.Г. Полякова. Минск: РНПЦ ОМР им. Н.Н. Александрова, 2020. С. 298.
References
1. Tlish MM, Kuznetsova TG, Sychev NL. Clinical and morphological aspects of carcinoid papillomatosis skin Gottron. Medical Herald of the South of Russia. 2014;2:138–143 (In Russ.). https://doi.org/10.21886/2219-8075-2014-2-138-143
2. Arsentev N, Bobkova A. Gottron’s Carcinoid Papillomatosis of the Skin. J Cutan Med Surg. 2023;27(5):541. https://doi.org/10.1177/12034754231193748
3. Pătrașcu V, Enache O, Ciurea R. Verrucous Carcinoma — Observations on 4 Cases. Curr Health Sci J. 2016;42(1):102–110. https://doi.org/10.12865/CHSJ.42.01.15
4. Kobernik MYu, Elkin VD, Sedova TG, Zhukova AA Case of development of Gottron’s carcinoid papillomatosis of skin against a background of protracted psoriasis. Perm Medical Journal. 2019;36(6):76– 82. https://doi.org/10.17816/pmj36676-82
5. Senanayake J, Chaudhari S, Haji Rahman R, Madanat S, Tiesenga F. Chronic Venous Insufficiency and Lymphedema With Papillomatosis Cutis Lymphostatica, Hyperkeratosis, and Skin Ulcers: A Case Report. Cureus. 2023;15(2):e35326. https://doi.org/10.7759/cureus.35326
6. Silva JA, Mesquita Kde C, Igreja AC, Lucas IC, Freitas AF, Oliveira SM, Costa IM, Campbell IT. Paraneoplastic cutaneous manifestations: concepts and updates. An Bras Dermatol. 2013;88(1):9–22. https://doi.org/10.1590/s0365-05962013000100001
7. Fania L, Didona D, Di Pietro FR, Verkhovskaia S, Morese R, Paolino G, Donati M, Ricci F, Coco V, Ricci F, Candi E, Abeni D, Dellambra E. Cutaneous Squamous Cell Carcinoma: From Pathophysiology to Novel Therapeutic Approaches. Biomedicines. 2021;9(2):171. https://doi.org/10.3390/biomedicines9020171
8. Murphy ES, Leyrer CM, Parsons M, Suh JH, Chao ST, Yu JS, Kotecha R, Jia X, Peereboom DM, Prayson RA, Stevens GHJ, Barnett GH, Vogelbaum MA, Ahluwalia MS. Risk Factors for Malignant Transformation of Low-Grade Glioma. Int J Radiat Oncol Biol Phys. 2018;100(4):965– 971. https://doi.org/10.1016/j.ijrobp.2017.12.258
9. Jin Y, Qu C, Shi T, Wang C, Yu H, Zhang F. A case of vegetative pyoderma gangrenosum. Dermatologica Sinica. 2015;33(3):170–172. http:// dx.doi.org/10.1016/j.dsi.2014.12.009
10. Ghosh S, Aggarwal K, Jain VK, Chaudhuri S, Ghosh E, Arshdeep. Tuberculosis verrucosa cutis presenting as diffuse plantar keratoderma: an unusual sight. Indian J Dermatol. 2014;59(1):80–81. http://dx.doi.org/10.4103/0019-5154.123511
11. Brito AC, Bittencourt MJS. Chromoblastomycosis: an etiological, epidemiological, clinical, diagnostic, and treatment update. An Bras Dermatol. 2018;93(4):495–506. http://dx.doi.org/10.1590/abd18064841.20187321
12. Bonnetblanc JM, Bédane C. Erysipelas: recognition and management. Am J Clin Dermatol. 2003;4(3):157–163. http://dx.doi.org/10.2165/00128071-200304030-00002
13. Vignes S. Les lymphœdèmes : du diagnostic au traitement [Lymphedema: From diagnosis to treatment]. Rev Med Interne. 2017;38(2):97–105. French. http://dx.doi.org/10.1016/j.revmed.2016.07.005
14. Karacheva IuV, Guzeĭ TN, Gladkikh LN, Larina TM. Gottron’s cutaneous Carcinoid papillomatosis. Klinicheskaya Dermatologiya i Venerologiya. 2017;16(3):29–35 (In Russ.). https://doi.org/10.17116/klinderma201716329-34
15. Arsentev N, Bobkova A. Gottron’s Carcinoid Papillomatosis of the Skin. Journal of Cutaneous Medicine and Surgery. 2023;27(5):541. http://dx. doi.org/10.1177/12034754231193748
About the Authors
T. I. BalabanovichBelarus
Tatsiana I. Balabanovich — Cand. Sci. (Med.), Assoc. Prof. of the 1st Department of Internal Diseases.
Gorkogo str., 80, Grodno, 230009
K. M. Surmach
Belarus
Katsiaryna M. Surmach — Cand. Sci. (Med.), Assoc. Prof., Associate Professor of the Department of Propaedeutics of Internal Diseases.
Gorkogo str., 80, Grodno, 230009
S. N. Dziamidzik
Belarus
Sviatlana N. Dziamidzik — Cand. Sci. (Med.), Assoc. Prof., Associate Professor of the Department of Phthisiopulmonology.
Gorkogo str., 80, Grodno, 230009
V. V. Budrevich
Belarus
Volha V. Budrevich — physician in the emergency department of the health care institution “Lida Central Regional Hospital”.
Mitskevicha str., 1, Lida, 231300
R. S. Warnakulasuriya Fernando
Belarus
Warnakulasuriya Fernando Rashina Shanani — student.
Gorkogo str., 80, Grodno, 230009
Supplementary files
Review
For citations:
Balabanovich T.I., Surmach K.M., Dziamidzik S.N., Budrevich V.V., Warnakulasuriya Fernando R.S. Gottron’s Carcinoid Papillomatosis: Case Report. Kuban Scientific Medical Bulletin. 2023;30(6):81-88. https://doi.org/10.25207/1608-6228-2023-30-6-81-88








































